The Symptoms and Diagnosis of Testicular Cancer
Testicular cancer is a rare form of the disease, but it's the most common cancer in men ages 20 to 40 and the second most common cancer in men ages 35 to 39. The average age of men who get a testicular cancer diagnosis is 33, so younger guys need to take note.
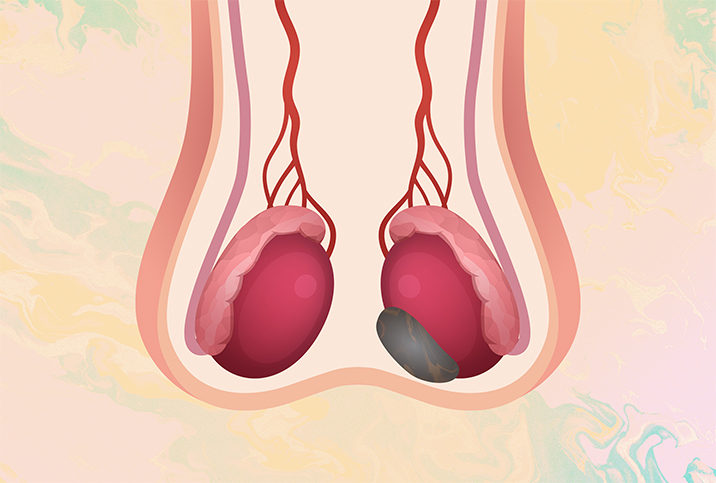
In almost all cases of testicular cancer, only one testicle is involved—but notice we said "almost all." There are instances where both testicles contain cancerous tumors.
Testicular cancer is often curable if it is detected, diagnosed and treated early: The five-year relative survival rate for men who are diagnosed with stage I (the earliest stage) testicular cancer is 99 percent. Here's the rub, though: Not all men with testicular cancer have easily identifiable symptoms. Most often, it will present early with a small, hard testicular lump.
Prostate exams are now a routine part of male health and wellness, but screening for testicular cancer is not always a part of annual checkups. Men of all ages—but particularly those between the ages of 20 and 40—should know the symptoms of testicular cancer and how testicular cancer is diagnosed.
Overview of testicular cancer
Testicular cancer develops when there are abnormal changes in a male's sperm cells, creating tumors in the testicle known as germ cell tumors. While there are currently no specific known causes for testicular cancer, its incidence rate has so dramatically increased over the last 20 years that researchers have begun looking at environmental and occupational factors that may contribute to the likelihood a man will develop testicular cancer. There may also be heredity factors, genetic mutations and birth defects that cause testicular cancer.
In the United States, testicular cancer is rare among Asian American, Black and Hispanic men. And while it's relatively rare for all men, Caucasian males have an up to five times greater risk of developing it than Black males and three times greater risk than Asian American males.
Globally, the testicular cancer risk is highest for European and American males and lowest for Asian and African males.
Treatment of testicular cancer is usually successful if the disease is in an early stage of development, and in almost all cases, treatment begins with the surgical removal of the germ cell tumor. If the cancer is localized—that is, it has not spread outside of the testicle—no further treatment may be needed.
If the cancer has spread outside of the testicle, however, then additional treatment after surgery will be necessary, depending on whether its spread is regional or distant. The oncologist overseeing the testicular cancer treatment will determine whether radiation or chemotherapy or a combination of the two should be used.
Cancer that has spread regionally from the testicle (to adjacent structures or lymph nodes) will likely be treated with targeted radiation first. However, if the cancer has spread distantly (to the lungs, neck, and armpits), then chemotherapy will likely be the next form of treatment after surgery.
Both radiation and chemotherapy come with risks that may affect both sexual and overall health. Radiation therapy may affect sperm count and quality, which could affect fertility. Chemotherapy for testicular cancer is usually successful because germ cell tumors are especially sensitive to it, but it might produce uncomfortable or life-threatening side effects. Tumors confined to the testicle will be primarily treated with an orchiectomy
Men who will be receiving radiation or chemotherapy for testicular cancer should discuss possible side effects with the oncologist overseeing their treatment.
The importance of testicular self-exams
The key to a successful outcome with testicular cancer is early detection, diagnosis and treatment. You should conduct a testicular self-exam once a month, so you can identify small changes quickly and bring them to your primary care doctor's attention immediately. While some small changes may be normal, others may not be.
Doing a testicular self-exam starts with knowing your anatomy, but there are a couple of things you should be aware of.
First, it is normal for one testicle to hang lower or be larger than the other testicle. Second, each of your testicles is lined in the back and on the top with a tube-like structure called the epididymis. This structure, which is bumpier and softer than the rest of your testicle, is where your sperm learn to swim.
To perform a testicular self-exam, do the following:
-
Take a warm shower. Warm water makes the exam easier because it relaxes the scrotum and the muscles that hold your testicles.
-
Gently roll the skin on each side of your scrotum with your fingers so you can feel the surface of your testicles to see if there are any bumps, lumps or anything else unusual present. Be aware of changes in the size of your scrotum and testicles since swelling can be a sign of testicular cancer.
-
Take note if your testicles feel heavy or have a dull ache in them, as this can also be a cause for concern.
If you find anything unusual during your testicular self-exam, schedule an appointment with your primary care doctor as soon as possible.
Testicular cancer symptoms
In many cases of testicular cancer, the only presentation is a painless, hard mass. But if you are experiencing pain, a dull ache or heaviness in one of your testicles, this is a good indication that one or more germ cell tumors may be growing rapidly.
About 30 percent of men who have testicular cancer don't seek treatment until they experience symptoms associated with metastatic cancer, which appear after the cancer has spread to distant regions of the body. For example, an abdominal mass may indicate the cancer has spread from the testicle to the lymph nodes that sit in your abdominal cavity behind the intestine. Also, persistent lower back, side or abdominal pain may be an indication that the cancer has spread to or is obstructing muscles, blood vessels or ureters.
If the cancer has invaded the inferior vena cava (IVC) or caused blood clots to form, you may experience swelling in your legs. If the cancer has spread to your lungs, you may have a persistent cough, difficulty breathing and chest pain.
In rare cases, men who are seeking help for infertility may be diagnosed with testicular cancer.
Other symptoms of testicular cancer include:
-
Night sweats and fever
-
Enlarged or tender breasts
-
Weight loss
-
Bloody sputum
-
Acute epididymis (the tube in the testicle that carries sperm) inflammation
Methods of diagnosing testicular cancer
Doctors can use any of several methods to diagnose testicular cancer. Usually, if there's an indication cancer may be present, your primary care doctor will refer you to a urologist. The urologist will first have a scrotal ultrasound performed, which will enable them to see any masses inside your testicles. Any such mass or masses are known as the primary tumors of your cancer, even if it has spread regionally or distantly.
Only a few types of cancers have tumor markers associated with them, and testicular cancer is among them. Tumor markers help establish your diagnosis, prognosis and treatment, and they will be monitored during your treatment since they are one (not the only) indicator of whether your cancer is responding to treatment.
Tumor markers that are initially assessed and continually monitored are alpha-fetoprotein (AFP), human chorionic gonadotropin (hCG) and lactate dehydrogenase (LDH).
Typically, when testicular cancer is found, your oncologist will order a full-body CT scan to see whether the cancer has spread and metastasized in other parts of the body. This scan will help the oncologist stage your cancer and determine treatment.
To confirm the diagnosis of testicular cancer, the entire testicle is surgically removed. Why the entire testicle and not just the tumor? If just the tumor is removed, the likelihood is high the cancer will spread and alter your body's lymphatic drainage patterns. Therefore, removing the testicle is more likely to lead to a better outcome, especially if the tumor is still confined to that testicle.
Testicular cancer typing and staging
Men can develop one of two types of testicular cancer: seminomas and nonseminomas. Germ cells in seminomas become malignant early in their development and are most likely to affect men in their 40s. Classic seminomas account for 85 percent of seminomas. Anaplastic seminomas spread aggressively and are more prone to metastasizing throughout the body. The other 15 percent of seminomas are spermatocytic, which most often develop in men over 50 and rarely metastasize.
The second type of testicular cancer is nonseminoma, which typically develops in men in their mid-30s. The two types of nonseminomas—embryonal carcinomas and yolk sac tumors—are aggressive and account for approximately half of all nonseminoma occurrences.
So those are the types of testicular cancer. Now let's explore its three stages. Stage I means the cancer is confined to the testicle and has not spread outside of it (localized). Stage II means the cancer has spread to other parts of the body, usually the abdominal lymph nodes adjacent to the testicle (regional). Stage III means the cancer has spread beyond the lymph nodes and has metastasized in other parts of the body, which may include the lungs, liver, bones and brain (distant metastatic disease).
Men with stage I testicular cancer have the best five-year relative survival rate: 99 percent. The five-year relative survival rate of men with stage II is slightly lower, at 96 percent. Men who have been diagnosed with stage III testicular cancer have the lowest five-year relative survival rate, at 73 percent.
Prevention of testicular cancer
Since research hasn't solidly identified any known causes for testicular cancer, there are no prescribable steps you can take to prevent developing it. However, you can be proactive in minimizing the impact of testicular cancer by conducting monthly testicular self-exams and keeping annual health and wellness appointments with your primary care physician.
A testicular cancer diagnosis is scary, but with early detection and solid medical care, you can survive and thrive despite it.