The Staging Methods of Testicular Cancer, Decoded
Receiving a diagnosis of testicular cancer is alarming. But once you get used to the idea—as much as possible—you have to talk about staging with your urologist or oncologist. This process is deeply distressing and also confusing.
The stage of cancer describes how much cancer is in the body, according to the American Cancer Society. Staging, in its simplest terms, gives both physicians and patients a good idea of the severity and spread of the cancer, survival rates and, ultimately, the course of treatment.
Most people have a general idea about what the stages of cancer denote: Stage I means the cancer was detected early, while stage IV means it has spread to other areas of the body.
Testicular cancer can be categorized by three different staging systems, or methods, said oncologist Jason Sager, M.D., CEO and president of Sagely Health in Boston. They're not at all effortless to understand.
The first method is descriptive, he said, with stages called local, regional and advanced (also called distant) cancer.
The second method is the American Joint Committee on Cancer (AJCC) system, which begins at stage 0 and goes to III (there is no IV) and further uses A (good), B (intermediate) and C (poor) substages. They look like this: 0, I, IA, IB, IC, II, IIA, IIB, IIC, III, IIIA, IIIB, IIIC.
TNM (tumor, lymph node, metastasis), the third method, is often used in conjunction with the AJCC method. The TNM system further elaborates the spread of the cancer, describing the tumor size (T); the number and size of involved lymph nodes (N); whether there is metastasis, or spread, of the tumor outside of the testicle (M); and, with a fourth designation of S, the serum (blood) levels of tumor markers.
Numbers follow the letters, indicating severity. For instance, an N1 designation means the cancer has spread to one lymph node; N3 means three lymph nodes, and so on. For M, or metastasis, and S, serum levels, the numbers are similarly indicative. If the number is 0, nothing has occurred yet, but if a higher number follows, then there's been relative growth or elevation of the cancer.
Staging, in its simplest terms, gives both physicians and patients a good idea of the severity and spread of the cancer, survival rates and, ultimately, the course of treatment.
But for M and T, staging actually occurs in, well, stages. This makes it sound even more complicated.
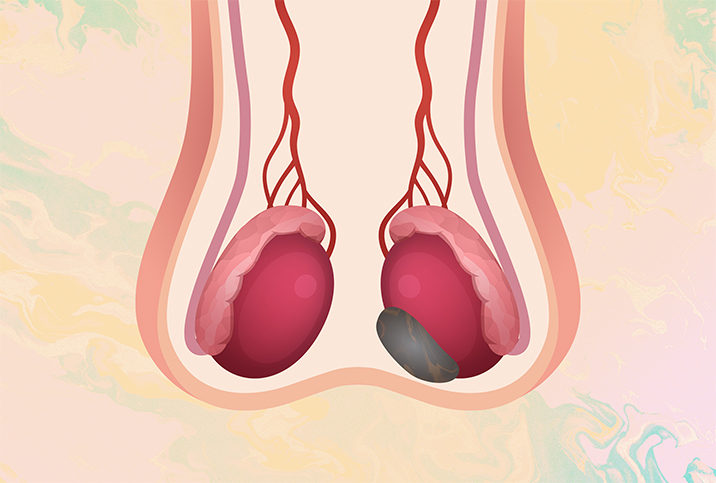
"Generally, after a testicular ultrasound confirms the presence of a mass in the testicle, the patient is scheduled for an orchiectomy to remove the cancerous testicle," said Mark Kantrowitz, an 18-year survivor of stage III seminoma, a type of testicular cancer. "The testicle is sent to pathology to evaluate the type of cancer—seminoma or nonseminoma—and, if the latter, the type of nonseminoma."
Doug Bank, a testicular cancer survivor, explains the tests used for staging on his Testicular Cancer Resource Center website: "Clinical staging uses radiological and physical clues to estimate the stage. Pathological staging uses stronger evidence, like tissue samples and blood tests, to determine the stage."
Based on an initial ultrasound and exam, but before an orchiectomy, the tumor size is referred to as cT. The c stands for clinical findings on a physical exam. After the surgery is performed, it changes to pT, which means the tissue has undergone cellular examination. Then the numbers 1 through 4 are assigned, based on what's discovered.
Finally, to make it even more confusing, the letter X might follow any of the cT, pT, N, M or S letters. X means there isn't enough information to fully assess these factors.
After the orchiectomy, an example of staging of testicular cancer might look like: stage IIA pT1 N1 M0 S0. This is a relatively good diagnosis, meaning the cancer has reached just one lymph node (N1) and hasn't appeared in distant parts of the body (M0), and tumor marker levels in the blood are normal (S0).
"Keep in mind that staging is only as accurate as the information available, and the stage of a person's cancer can change as more information or more accurate information is gathered," Bank wrote on his website. "If the doctor comes out of the operating room and tells you he thinks he got it all, don't be so quick to believe him. It takes urologists, pathologists and radiologists to ultimately determine the stage of the cancer."
When it comes right down to it, however, how much of the technical lingo does a testicular cancer patient really need to know? Only the basics, Sager said.
"The AJCC and TNM staging methods are complicated and unlikely to be impactful for testicular cancer patients, so it would not be particularly beneficial for them to study it thoroughly," he said.
A patient's overall health is a dominant factor "when interpreting the severity of the disease," Sager said.
In fact, he emphasized he uses the first method, the descriptive one, when talking to patients because the local, regional and advanced designations are easier to understand and translate into more practical outcomes. However, staging also involves understanding risk and treatment, so he reverts to those other methods for more advanced testicular cancer patients.
"It is fairly easy to understand the value of monitoring a relevant blood-circulating tumor marker throughout treatment," Sager added, referring to the S of the TNM system. "When the number decreases, it usually indicates the cancer is responding to treatment. If the number increases significantly, then the cancer may have returned or be growing."
He cautions that no system is perfect, so it's important to have the patient's oncologist interpret the staging findings, too.
The type of cancer and its aggressiveness are also important factors, said Kantrowitz, who runs cancerpoints.com, which offers practical tips for cancer patients, survivors and their families. The patient's age needs to be considered. A patient's overall health is a dominant factor "when interpreting the severity of the disease," Sager said.
Sager recommends getting additional opinions whenever possible.
"There are usually several options to consider even within a specific stage. Rather than try to evaluate the different options on their own, I recommend that all cancer patients get a second opinion, preferably at an NCI-accredited comprehensive cancer center," he said, referring to the National Cancer Institute.
He called it a no-lose step for almost all patients, because "nearly all second opinions are covered by insurance."
This is where Kantrowitz's and Bank's websites for testicular cancer patient advocacy come in handy. Bank's site noted that in 2018, there were 11,000 practicing urologists in the United States. This is significant because it means there are more urologists in the country than testicular cancer patients, who number 8,000 to 10,000 each year.
"In other words, even the doctors who are supposed to know the most about TC may not see it very often," Bank wrote on his site, where you can find lists of urologists and pathologists who specialize only in testicular cancer.
Sager, a patient advocacy supporter at Sagely Health, agreed specialization is essential for treating testicular cancer, a relatively rare disease. Find an expert—or two—who will explain the technicalities in staging and treatment in clear language rather than medical lingo. Then you can decide on a specific course of action that maximizes your chances of survival.

















