Why Is Advanced Prostate Cancer on the Rise?

A look at the big picture of cancer prevention is a positive one: Diagnosis and treatment and advances in fighting the disease over the past couple of decades have been pretty incredible.
Efforts by various healthcare societies, government agencies and front-line providers have yielded stunning results. Overall, cancer mortality has dropped 33 percent since 1991, according to the American Cancer Society (ACS).
For male-specific cancers, the news is largely positive. The five-year relative survival rate for testicular cancer is 95 percent, while it's 96.8 percent for prostate cancer, according to U.S. government data.
However, some bad news is mixed in with the good. A new study published by the ACS in its Cancer Facts & Figures 2023 report shows that for the first time in 20 years, the rate of men presenting with cases of advanced prostate cancer is increasing.
With such tremendous recent progress on cancer in general, as well as the progress specific to prostate cancer, what's to explain the sudden turnaround in terms of advanced prostate cancer? Experts have some thoughts.
What's going on here?
Analysis of the data in the ACS report suggests that prostate cancer cases rose 3 percent per year from 2014 to 2019. This increase in overall prostate cancer cases appears to reflect a 4 percent to 5 percent annual rise in cases of advanced-stage prostate cancer that's either regional or distant stage, meaning cancer that has spread to other parts of the body.
The subset of men diagnosed with distant-stage prostate cancer has doubled during that same period.
Experts suggest one possible cause may be recent changes in screening recommendations.
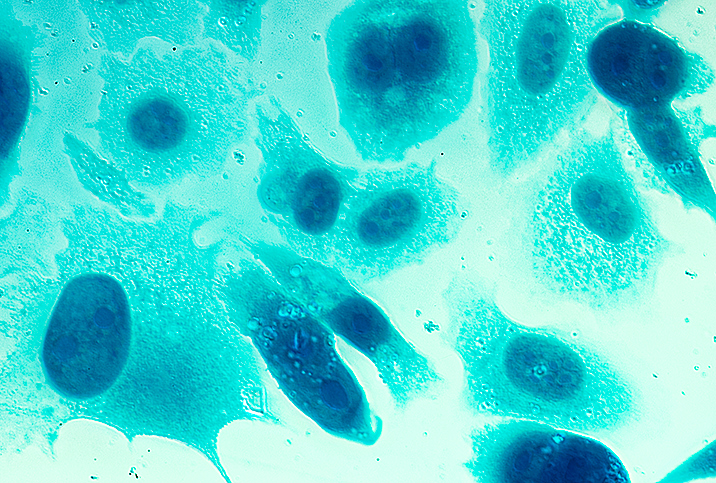
There was concern years ago about overdiagnosis and overtreatment for prostate cancer based on screening with the prostate-specific antigen (PSA) test. PSA is a protein that's produced by both healthy and cancerous cells in the prostate gland but is produced in higher concentrations when cancer is present. Based on their PSA results, among other criteria, some men who didn't actually have aggressive, fast-growing prostate cancer may have been subjected to stressful, painful biopsies and even unnecessary prostatectomies.
The recommendations for PSA testing have been the subject of debate in recent years.
"What's happened is because of the [PSA's] wide use, we essentially performed more biopsies and more treatment," said Jayram Krishnan, D.O., a urological oncologist whose practice is affiliated with Cleveland Clinic. "So now the urology community has scaled back in terms of realizing not every prostate cancer requires treatment. There was essentially overtreatment that was performed for prostate cancer, and prostate cancer treatment is not free, so to speak. There are side effects with any of the treatments."
In 2018, the U.S. Preventive Services Task Force (USPSTF) published research with the conclusion that PSA testing may have led to significant harm, despite potentially preventing about 1.3 deaths from prostate cancer per 1,000 men (ages 55 to 69) screened over 13 years and three cases of metastatic prostate cancer per 1,000 men screened.
Harm associated with screening includes undue anxiety from false-positive results, unneeded biopsies and their complications, and even unneeded prostatectomy surgery, all of which may reduce the quality of life for a number of men.
One of the USPSTF recommendations was that PSA screening should be an individual decision for men ages 55 to 69 who are at average risk, and these men should discuss screening with their healthcare providers.
Some people in the medical community suspect this recent rise in advanced prostate cancer cases may be related to fewer men choosing to be screened.
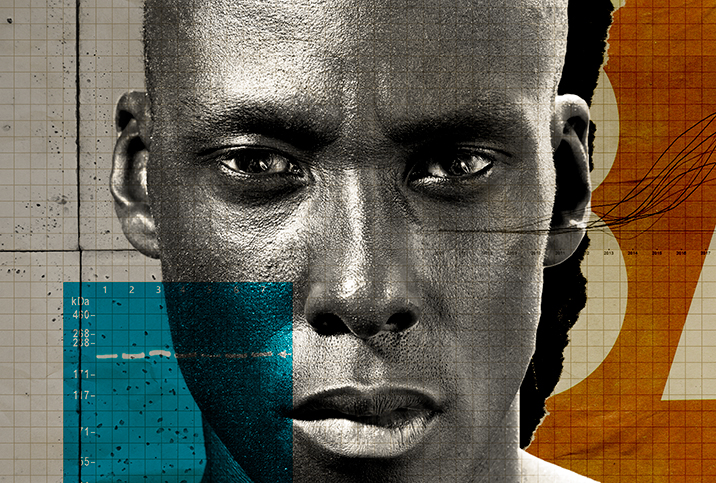
"I do believe that the lack of screening—it's circumstantial—but I do believe it has led to an increase in metastatic disease," said Daniel P. Petrylak, M.D., chief of genitourinary oncology at Yale School of Medicine. "We also wonder if the biology has changed somewhat. That's the other possibility, too, or some combination thereof: dietary fat, the obesity epidemic in the U.S., all these things come into play. There are alternatives."
What's to be done
One wrinkle in the story of changing PSA testing recommendations is that these days, many of the concerns about overtreatment and the like are no longer as relevant.
For one thing, providers, pathologists and oncologists have much more developed resources in terms of assessing what constitutes a dangerous, fast-growing cancer. More slow-growing types—for instance, cancers with a low Gleason score, such as a 6—can often be monitored.
The "kill it with fire" approach to each and every sign of prostate cancer is largely a thing of the past.
"What I think has actually happened is that, with the treatment of Gleason 6—the prostate cancer you die with, not die from—more watchful waiting is being done," Petrylak said. "So that morbidity issue is starting to become a little bit less important than it was before."
For most providers, the main takeaway from the ongoing PSA testing debate is realizing that there just isn't a one-size-fits-all protocol for any patient. The patient's age, overall health, genetic predisposition to prostate cancer—African American men are at a much higher risk, for instance—and other factors must all be considered.
"It should really be based on how long do you think your patient is going to live and what are the risk factors for them developing prostate cancer," Petrylak said. "If you've got somebody that's 90 years old, you should really question whether you're going to screen this guy or not. If they develop symptoms or have issues, that's one thing, but just random screening? I'm not sure it's worth it at that point.
"This requires a very clear discussion of what the patient's goals are and what they want in terms of quality of life. There's a lot that goes into it," he added.
Conclusions
The slight bump in cases of metastatic prostate cancer likely has multiple causes, but the PSA testing issue could very well be among them.
Luckily, the medical community has made great strides in not only diagnosing and differentiating various levels of prostate cancer but also in opening up patient-provider discussions. Making sure the patient's goals and individual health and quality of life concerns are centered is paramount.
"Basically, there's a lot more partnership with the physician, a lot more discussion," Krishnan said. "It's not like, 'OK, your PSA is slightly high, you're going to get a biopsy and, ultimately, have treatment.' It's not set in stone anymore."
Are you getting to the age where screening—or at least a discussion about screening—is recommended by the USPSTF? Have a conversation with your doctor about a PSA test. If you don't have a regular physician, now is the time to find one. Giddy Telehealth takes the difficulty out of such a search, providing access to hundreds of healthcare professionals who offer video visits as a regular part of their practices. It is an easy-to-use online portal whose physicians, therapists and others have expertise across the full scope of medical care. Many have same-day appointments.