Don't Phone In Your Sexual Health

While many medical providers have been forced to rely on remote and telehealth appointments at intermittent points during the past year, the easing of restrictions in response to mass vaccination and an overall decline in COVID-19 cases raises the question: When can people begin seeing doctors and counselors in person regularly? And, more importantly, what does that mean for my sexual health?
Sexual health screening and in-person counseling are just a couple of the issues to consider in regard to a return to our old medical and health practices.
Here's a refresher about a few things you may not have thought very much about over the past year.
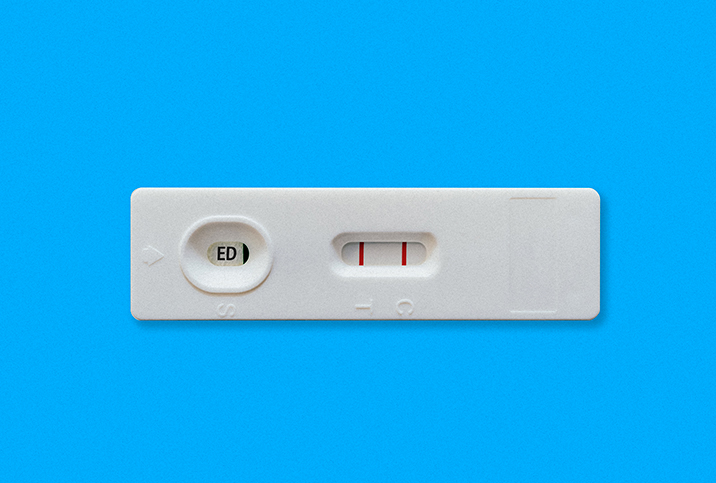
Get lucky? Get tested
As the coronavirus dominated most of the testing carried out over the past year, it seems important to acknowledge and remind ourselves of basic best practices and considerations regarding our sexual health and wellness:
- Abstaining from sexual contact is the only 100 percent effective method of preventing the transmission of sexually transmitted diseases or infections (STDs/STIs).
- Used correctly, barrier protection methods can be highly effective at preventing the transmission of HIV/AIDS, syphilis, gonorrhea and other diseases.
- Certain lifestyles and sexual behaviors have an increased risk of disease transmission, unwanted pregnancy and other complications. If you have concerns about a particular sexual practice, you should consult your doctor about options such as PrEP, a strategy of medicines that can help prevent the contraction of HIV.
- Similarly, it's important to talk to your doctor about birth control options and any negative experiences you may have had related to taking birth control. Not all birth control options are right for everybody, and you should weigh potential side effects against the benefits.
- Regular testing is critical. Many sexually transmitted conditions can be asymptomatic for extended periods, and when symptoms do occur, their presentation can vary wildly in terms of timing and intensity. In the time it takes for symptoms to present, a person could unwittingly have infected multiple partners.
Only a medical professional can advise you on best sexual health practices, but even a qualified medical team can't make adequate recommendations without you providing the necessary background data, so have that ready.
Communicate with your partner(s)
Your partner(s) needs information, too.
While the topic may not feel particularly sexy to bring up during foreplay, sex is so much better when it's done with informed consent. However, your partner can't provide consent if they haven't been informed about what they are consenting to, including any infections you have, what protection you (or they) want to use and what acts you will, won't or want to do.
Does this mean you need to have a detailed list of your sexual partners and practices during your entire lifetime? Of course not. But revealing recent sexual history, along with practices regarding protection, can provide peace of mind and an enhanced bonding opportunity between partners or potential partners.
Just remember, any sexual activity comes with a certain degree of risk, and a conversation, however honest, doesn't necessarily guarantee safety. The hard truth is people can be dishonest about their STD/STI status or simply misinformed for any number of reasons. This is why the importance of regular STD/STI screening can't be overemphasized.
Convenience isn't comprehensive
The things people miss from in-person appointments will be a little bit different from person to person. Some may want to continue to conduct most of their health appointments remotely. If they can achieve comprehensive health management while maintaining the status quo of pandemic primary healthcare, then good for them.
However, let's not forget that people need real support in dealing with some health issues, whether they be sexual, mental or physical. It's hard to justify remote health as standard practice if there is any chance it could lead to increased marginalization of national issues relating to sex, physiological conditions or mental health.
Health outside the doctor's office
We've all been through a lot over the past 18 months. The losses are still devastating and, like it or not, our entire way of life has changed.
We're not quite in the clear yet, but things are looking and feeling good right now. If you're ready to start getting back out there, make sure you're working with your doctor(s) and your partner(s) to do it the right way.