Gonorrhea is the second most common sexually transmitted disease (STD) in the United States. The Centers for Disease Control and Prevention (CDC) estimates there were about 1.6 million new gonorrhea infections in 2018. However, that statistic comes with the caveat that fewer than half of these infections are actually reported to the CDC.
The Facts About Gonorrhea
Find out how gonorrhea affects your sexual health.
What is gonorrhea?
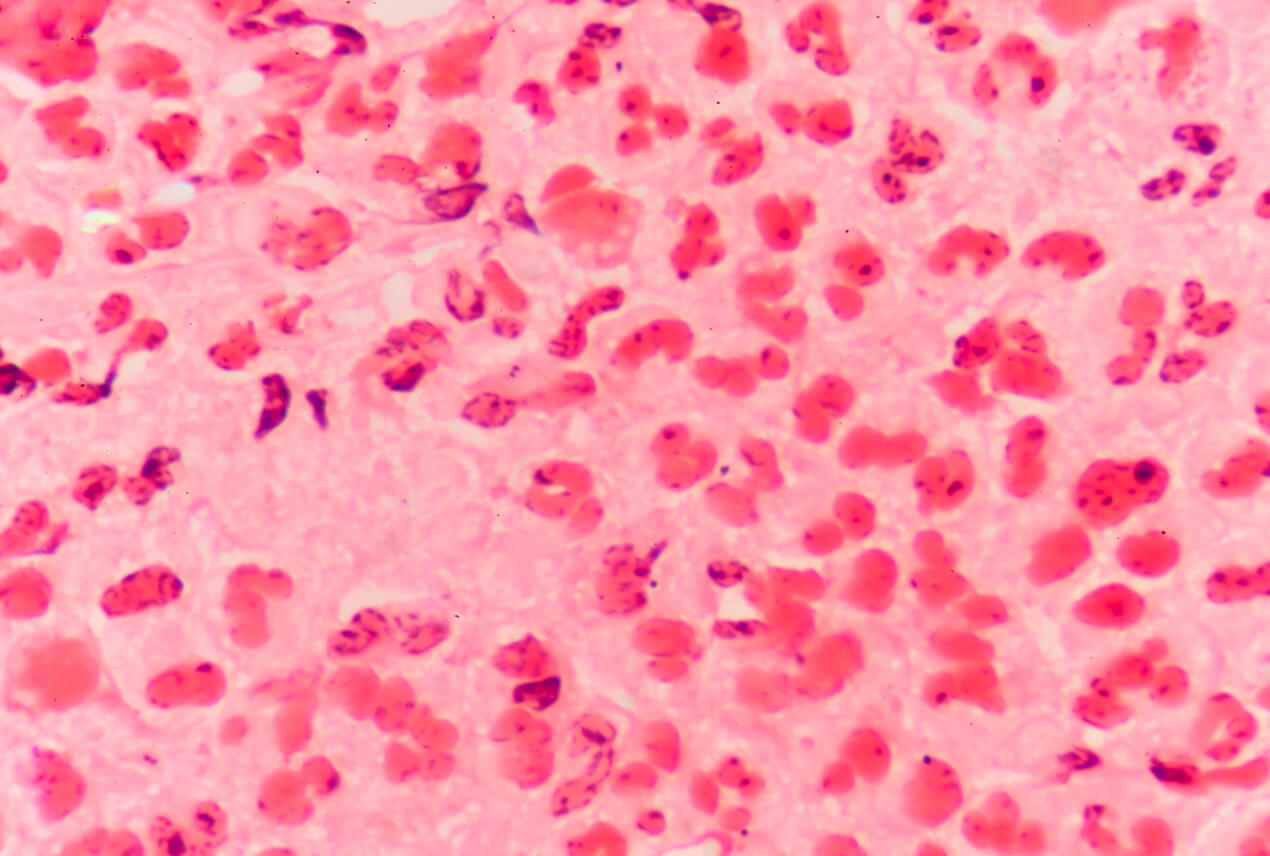
Gonorrhea, a bacterial infection caused by the bacteria Neisseria gonorrhoeae, is a disease transmitted through unprotected sex that affects the penis, vagina, anus or mouth.
Untreated gonorrhea flourishes in warm, moist areas of the body, such as the vagina, urethra, throat, anus, eyes and even the fallopian tubes, uterus and cervix. Left untreated, the STD can lead to complications such as lasting damage to the urethra and testicles.
Risks
Left untreated, gonorrhea can lead to a host of symptoms and complications, including infertility, infection, and an increased risk of contracting another sexually transmitted infection (STI) or a virus such as HIV. Complications and severe symptoms are easiest to avoid when the infection is detected and treated early.
Medical experts report that sexually active women younger than 25, men who have sex with men, and individuals with multiple sexual partners are at greater risk for contracting gonorrhea. Additionally, you are at greater risk for the infection if you already have a history of contracting other STDs.
Symptoms
Gonorrhea symptoms can range in severity from mild to severe and typically emerge within two to 14 days of exposure, though some people may experience no symptoms.
Common symptoms of gonorrhea include:
- Abdominal or pelvic pain
- Anal itching or pus-like discharge
- Increased vaginal discharge
- Painful urination
- Pus-like penile discharge
- Rectal bleeding
- Testicular swelling or pain
- Vaginal bleeding after intercourse
- Vaginal bleeding between periods
Many people develop asymptomatic gonorrhea, so it can be difficult to detect and, therefore, easier to unknowingly spread. If you have unprotected sex, a history of contracting STIs or multiple sexual partners, you should undergo regular screenings to ensure that any potential infections are detected and treated early.
Diagnosis
The most common way a doctor can determine if you have gonorrhea is with a urine test that can reveal whether the bacteria Neisseria gonorrhoeae is present in your urethra. If potential symptoms are present, the doctor can take a swab of whichever area is affected—throat, urethra, vagina, eyes, rectum—and have it tested in a lab.
Mayo Clinic reports that women can use home kits to test for gonorrhea. They involve vaginal swabs that are then sent to a lab for testing.
If you think you may be experiencing symptoms of gonorrhea, get tested immediately to avoid severe symptoms and complications. If you think you're at risk, most doctors recommend getting screened for common STDs on a quarterly basis to increase early detection and treatment and to lessen the spread of infections.
How is gonorrhea spread?
Since it is sexually transmitted, gonorrhea is spread through many types of sexual activity, such as unprotected vaginal, anal or oral sex. Once transmitted, gonorrhea can affect the urethra, rectum, throat, cervix, fallopian tubes and even the eyes and joints.
Though gonorrhea is spread primarily through unprotected sex, an untreated infection can also be spread from mother to child during childbirth. Infected newborns can develop serious symptoms and permanent complications, including blindness, if the infection is left untreated.
Research
According to recent research, the prevalence of gonorrhea is at an all-time high in the U.S. In fact, CDC numbers for 2018 (the latest statistics available) show that cases of gonorrhea—as well as chlamydia and syphilis—have skyrocketed.
Though gonorrhea is nothing new—reported infections date as far back as 200 B.C.E.—there has been much speculation as to what's causing such a marked increase in the number of cases. Public health researchers indicate it may be a confluence of circumstances, including the opioid crisis leading to more unsafe sex, the overall decline in condom use and funding cuts to national STD awareness programs.
Prevention
The best way to prevent the spread of gonorrhea is by practicing safer sex, especially if you have multiple sexual partners.
Sexual health experts recommend using a latex condom for protection. You should also switch to a new condom if you're transitioning from anal to vaginal sex or from anal or vaginal to oral sex. Gonorrhea can be transmitted orally, so protection is necessary for oral sex as well. You can use either a latex condom or, for greater comfort, you and your partner can use dental dams for protection.
To prevent the spread of gonorrhea and other STDs, annual routine STD screenings should be scheduled for nonpregnant adults who are at lower risk. For those in higher risk groups, STD screenings should be carried out every three months. Pregnant women should also be tested, as gonorrhea can be transmitted during childbirth.
If you or your partner are experiencing any potential symptoms of an STD, abstain from sex until you are tested and have received any necessary treatment.
Treatment
Gonorrhea is typically treated through antibiotics administered via injection. The type of antibiotic your doctor prescribes varies depending on which strain of gonorrhea you have. Some strains of gonorrhea are easily treated, while others are antibiotic-resistant—strains sometimes referred to as super gonorrhea.
Since more and more cases of gonorrhea have proved to be resistant to antibiotics, the CDC has recommended that uncomplicated gonorrhea strains be treated with an injection of an antibiotic called ceftriaxone. Alternative options are available for patients who may be allergic to ceftriaxone. Any sexual partners, whether they have symptoms or not, should undergo the same treatment.
Just like adults, babies who contract gonorrhea during childbirth are also treated with antibiotics.
If left untreated
All individuals can be left with serious and lasting health complications when gonorrhea goes untreated. Symptoms of untreated gonorrhea can lead to permanent scarring of the urethra and lasting damage to the testicles.
Pelvic inflammatory disease (PID) can develop in women if gonorrhea spreads to the uterus or fallopian tubes, which can lead to severe pain in the abdomen, fever, internal abscesses and long-term pain in the pelvis. Women who develop PID as a result of untreated gonorrhea are also at greater risk for infertility and ectopic pregnancy.
Untreated gonorrhea can cause epididymitis in men, which can potentially lead to infertility.
In severe cases of untreated gonorrhea, the infection can spread to the blood, causing disseminated gonococcal infection (DGI), which can lead to arthritis, dermatitis and more. Doctors consider DGI a life-threatening condition.
Gonorrhea and pregnancy
Gonorrhea exposes pregnant women to a host of risks:
- Premature birth
- Miscarriage
- Chorioamnionitis (infection of the membranes and amniotic fluid around the baby)
- Premature rupture of membranes
- Having a baby with a low birth weight
Gonorrhea also can be passed to the baby during childbirth. Fortunately, there is safe treatment available for pregnant women with gonorrhea. Treatment includes an intramuscular injection of an antibiotic called ceftriaxone. And in cases where an infant is infected, they can be treated with erythromycin or, if that is unavailable, ceftriaxone or cefotaxime.
It is crucial for people who are pregnant to be tested for the infection early because of the risks gonorrhea poses during pregnancy.
Gonorrhea and fertility
Gonorrhea can affect fertility in both men and women. A gonorrhea infection left untreated can cause swelling of a man's epididymis, which is a coiled tube located at the back of each testicle near the top. This can lead to epididymitis, which makes it more difficult for sperm to travel out of the testicles to fertilize an egg.
Fortunately, epididymitis can be treated with antibiotics, which can prevent future swelling of the epididymis.
While male infertility caused by gonorrhea can typically be reversed with treatment, that is not always the case for women. Pelvic inflammatory disease can develop as a result of untreated gonorrhea, leading to serious scar tissue on the fallopian tubes. The scar tissue can make it difficult, and sometimes impossible, for eggs to be properly fertilized. The CDC reports that about 12 percent of women with PID become infertile.
Gonorrhea and erectile dysfunction
It's not uncommon for a gonorrhea infection to lead to a man's inability to have an erection. Gonorrhea can lead to the development of epididymitis and prostatitis, conditions that can cause symptoms of erectile dysfunction (ED).
Epididymitis is a condition in which bacteria inflames the epididymis, the coiled tube at the back of each testicle that carries sperm. Men who have chronic epididymitis often experience ED.
Prostatitis, on the other hand, is a bacterial infection that causes inflammation and swelling of the prostate gland. Men with prostatitis may experience painful ejaculation, which can lead to erectile dysfunction.
Chronic cases of both epididymitis and prostatitis can lead to long-term struggles with ED because of the physical, and often psychological, discomfort that accompanies the conditions.
How gonorrhea affects other parts of your body
A common misconception about gonorrhea is that it affects only the genitals. In reality, gonorrhea can affect the rectum, throat, joints and eyes, because the bacterium that causes gonorrhea flourishes in parts of the body that are warm and moist.
Signs of anal and rectal gonorrhea can include anal itching, constipation, painful bowel movements, bleeding and abnormal discharge. Gonorrhea that affects the throat can cause a sore throat that doesn't go away and swollen lymph nodes in the neck.
When gonorrhea spreads to the eyes, it can cause symptoms such as redness, pain, swelling, light sensitivity, difficulty opening the eyes and abnormal discharge from the eyes. Gonococcal arthritis, a form of septic arthritis, is a painful infection in the joint caused by gonorrhea.
How do I know if I have gonorrhea?
The only way to know for sure if you have gonorrhea is to get tested. But don't wait until you experience signs or symptoms before going to the doctor for screening, because the reality is that many cases of gonorrhea present no symptoms at all. The longer gonorrhea goes undetected, the greater your chances are of developing severe health complications and the more likely you are to spread the disease to others.
FAQs
Does gonorrhea go away on its own?
Gonorrhea does not go away on its own and requires treatment to avoid serious health complications. This STD is typically treated through antibiotics administered via injection. Early detection and treatment are important to prevent health problems and reduce the spread of the disease.
What happens if gonorrhea is left untreated?
Untreated gonorrhea can lead to infertility in both men and women. While fertility may be restored with treatment for men, this isn't always the case for women. In severe cases of untreated gonorrhea, the infection can spread to the blood and cause disseminated gonococcal infection (DGI), which can lead to arthritis, dermatitis and more.
How is gonorrhea transmitted?
Gonorrhea, a bacterial infection caused by the bacteria Neisseria gonorrhoeae, is a disease transmitted through unprotected sex involving the penis, vagina, anus or mouth. A fairly common sexually transmitted disease, gonorrhea infected about 1.6 million people in 2018, according to the latest statistics from the CDC.












