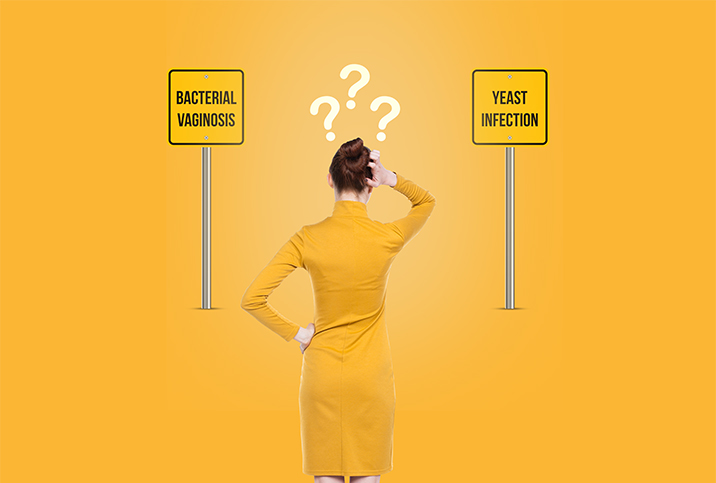
Bacterial Vaginosis vs. Yeast Infection: What's the Difference?
You know your vagina better than anyone. When something isn't quite right, you just know. It's important to listen to that instinct: While changes within the vagina are extremely common, they can also be a warning sign of a more serious condition.
Vaginitis, which refers to various conditions that cause inflammation and discomfort of the vagina, is often a culprit. Bacterial vaginosis (BV) and yeast infections are two of the most common types of vaginitis. These conditions can have similar symptoms, but they are not the same.
Understanding the differences between both will help you quickly identify the right treatment—so you can ditch the itch and speed up your recovery.
What are the causes?
Your vagina has a healthy mix of yeast and bacteria (both good and bad). When there's a disruption in their natural balance, it often leads to an overgrowth of the organism, resulting in vaginitis.
BV causes
The most common type of vaginitis, BV, affects nearly 30 percent of women at any given time, according to a 2007 study published in Sexually Transmitted Diseases. BV occurs when certain bad types of bacteria in the vagina grow more rapidly than the good bacteria.
"Women in their reproductive years are most likely to get bacterial vaginosis, but it can affect women of any age," said Maria Sophocles, M.D., a gynecologist and medical director at Women's Healthcare of Princeton, New Jersey. "While the cause of BV isn't completely understood, certain activities increase your risk."
Some common risk factors for BV include:
- Frequent douching
- Sudden hormonal changes that may alter your vaginal pH, such as pregnancy, menopause or menstruation
- New or multiple sexual partners
- Having sex without a condom
- Smoking
Yeast infection causes
A vaginal yeast infection, also known as vulvovaginal candidiasis, is a fungal infection caused by yeast overgrowth—often Candida albicans.
While it's normal for small amounts of this yeast to live in the vagina, certain events can lead to a disruption in their normal balance. This results in an overgrowth of yeast that leads to infection.
Yeast infection risk factors include:
- Major hormonal changes, such as pregnancy
- Hormonal contraceptives, such as birth control pills that increase estrogen levels
- Antibiotic use, which kills the natural bacteria found in the vagina
- A weakened immune system
- Diabetes
What are the symptoms?
Although some symptoms could point to either a yeast infection or BV, there are key differences to look for when distinguishing between the two. Vaginal discharge and smell are often the main identifying factors, so it's important to pay close attention to these.
BV symptoms
Bacterial vaginosis may not cause any noticeable symptoms, and those that do arise may resemble those of a yeast infection.
The most common BV symptoms include:
- Thin, gray, white or green vaginal discharge
- Foul, "fishy" vaginal odor
- Burning sensation or pain during urination or sexual intercourse
- Vaginal itching
Bacterial vaginosis will not cause the vulva to appear red or inflamed, as yeast infections will.
Yeast infection symptoms
Many times, a vaginal yeast infection presents itself with one or more easily identified symptoms such as itching or burning.
The most common yeast infection symptoms include:
- Thick, white discharge with chunky, cottage cheese consistency
- Vaginal pain and soreness
- Burning sensation or pain during urination or sexual intercourse
- Vaginal itching
- Redness and inflammation of the vulva
Notably, yeast infections will not change vaginal odor, like BV would. BV has a much higher than normal pH so an at-home pH test (although it won't deliver an official diagnosis) can help point you in the right direction.
Treatment options
Because BV and yeast infections are treated differently, it's important to get a proper diagnosis. Your doctor will make the determination.
BV treatment
There are no over-the-counter products available for BV, so it's best to visit your healthcare provider if you're experiencing symptoms—preferably a gynecologist but a primary care physician is knowledgeable in this department, too. BV is a bacterial condition and is easily treated with oral or vaginal (since they are absorbed through the mucosa) topical antibiotics.
Be mindful that BV does commonly recur within the first 12 months and may require a second round of antibiotics. While it's possible for BV to clear up without treatment, allowing it to go untreated can lead to serious complications:
- Preterm birth in pregnant women
- A higher risk of sexually transmitted infections
- Increased risk of infection following a gynecologic surgery
- Pelvic inflammatory disease (PID)
Yeast infection treatment
Although most yeast infections are mild, some cases can develop into more serious infections. Treatment for mild to moderate yeast infections often includes taking an antifungal medication, which includes creams, ointments and suppositories. You can find many of these medications over-the-counter (OTC) or by prescription.
Some may choose to start with OTC medication before visiting their healthcare provider. If symptoms persist after several days of treatment, it's best to visit your doctor for a proper evaluation.
When to visit a doctor
"When vaginal odor is strong enough to be unwanted, socially embarrassing or persistent, or the symptoms of itching and burning are not relieved by over-the-counter yeast preparations, it's time to visit a clinician," Sophocles said.
While the majority of bacterial vaginosis and yeast infection cases are mild, both conditions can result in more severe complications. To avoid potential issues, it's important to seek help from your doctor sooner, rather than later.
Your healthcare provider will likely perform a pelvic exam, take a sample of vaginal fluid or test your vaginal pH to help identify the problem. In most cases, you'll receive a diagnosis immediately, but lab tests may be ordered if your doctor is unsure. They may also rule out other possible causes, such as sexually transmitted infections.
Within two to three days of proper treatment, you should begin feeling better. Make sure you finish all medication, even if your symptoms clear up. If you don't, you may experience a recurrence of symptoms within weeks.
While both conditions appear similar, they are slightly different and require different treatments. Stay on top of your vaginal health and your groin region will thank you for it later.