What's the Link Between Bacterial Vaginosis and Menopause?

Bacterial vaginosis (BV) can develop when there's a change in the balance of bacteria in your vagina. It's a common condition that affects about 30 percent of women ages 14 to 49 and 1 in 4 pregnant women. However, most of the research on BV has been done on women who are premenopausal, meaning they're still menstruating and aren't having symptoms of perimenopause or menopause.
Normally, the vagina has a balance of both "good" and "bad" bacteria. This bacterial environment in your vagina is known as the flora, or microbiome.
"In a healthy vagina, the normal pH is acidic. A community of good bacteria called Lactobacillus within the vagina keeps it acidic and this helps ward off infections," said Ramya Sethuram, M.D., a reproductive endocrinologist at the Reproductive Science Center in the San Francisco area.
However, when bad bacteria start to overcrowd the good bacteria, it changes the pH balance in the vagina and can lead to certain infections, such as bacterial vaginosis.
Symptoms of BV, according to Sethuram, include vaginal burning or itching, burning when you urinate or a strong fishy odor. Your vaginal discharge might look white, gray or green in color. But some people don't experience any symptoms.
Despite the fact many women get BV from having sex, it's not considered a sexually transmitted infection (STI). However, having new or multiple partners or having sex without a condom can increase your chances of infection.
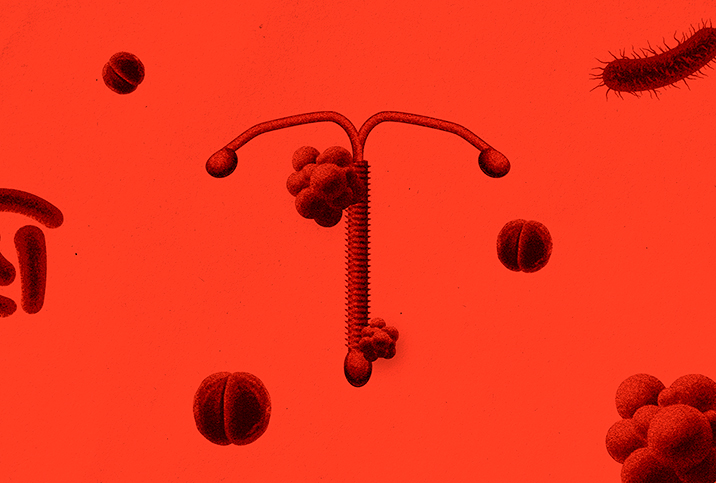
Even women who aren't sexually active can develop bacterial vaginosis. It's unknown exactly what causes BV, but certain factors besides having sex, including taking antibiotics, smoking tobacco or using an intrauterine device (IUD), can increase your chances of getting it.
Menopause and BV risk
According to Sethuram, your chances of getting a BV infection increase as you age, especially if you've had BV before.
Starting in your 40s, your reproductive system gradually begins to wind down and you enter a stage known as perimenopause. Your ovaries start making less estrogen and progesterone, and your periods can become more irregular as you approach menopause. Officially, if you've gone 12 months in a row without a period, you are considered to be in menopause.
"Premenopausal women typically have adequate ovarian function in which concentrations of estrogen and progesterone are high enough to protect and maintain a healthy vaginal flora with an acidic pH," said Monica Grover, D.O., a board-certified OB-GYN and the chief medical officer at VSPOT, a women's sexual health practice based in New York City. "The pH is important as it helps to protect healthy concentrations of Lactobacillus species, which are responsible for warding off any potential vaginal and urinary pathogens."
A balanced vaginal flora that contains both good and bad bacteria helps maintain this acidic environment, but estrogen also plays a role. As you age and make your way through menopause, decreasing estrogen levels can also lower your levels of beneficial Lactobacillus, according to Grover. This can make your body more vulnerable to vaginal and urinary tract infections (UTIs).
Lower estrogen levels push this acidic environment into a more alkaline one, which means Gardnerella vaginalis, the bacteria that cause BV, can overgrow, Sethuram said. These bacteria thrive in this less acidic environment and can cause irritation and inflammation in the vagina.
Sex during menopause with BV
It can be difficult to prevent BV because anything that upsets the delicate balance of your vaginal flora can cause the infection to come back. If you get a BV infection, there's an 80 percent chance you'll have another.
Generally, you don't have to stop having sex, but talk to your healthcare provider about it. If they give you antibiotics, take the entire course, unless you hear differently from your provider. But stay away from douching—good advice in general—as it can lower your good bacteria levels. Sethuram also recommended safer sex practices—use a condom even if you're in menopause and aren't concerned about pregnancy—if you continue to have problems with recurring BV.
If you're having BV symptoms in menopause, talk with your healthcare provider about treatment. If you have a male partner, they don't need to be treated, but if you are having sex with a female partner, they should be treated if they have symptoms.
According to Sethuram, 80 percent to 90 percent of BV infections can be cured within a month by using oral or intravaginal antibiotics such as metronidazole and clindamycin.
In some cases, BV goes away on its own without treatment, but it's still a good idea to address your individual symptoms with your provider. If you have an active BV infection, it's probably best to refrain from sexual activity until your symptoms clear or you complete antibiotic treatment.
Bacterial vaginosis can happen more often in women in menopause because of the change in hormone levels. Falling estrogen and progesterone production can upset the pH balance of the vagina and cause an overgrowth of bad bacteria. Talk with your healthcare provider about the steps you can take during menopause to decrease your chances of a BV infection.