How Being Low-Income Impacts Reproductive Healthcare

Low-income women face barriers to accessing many forms of basic reproductive healthcare. Reproductive healthcare can encompass routine gynecological exams, sex ed, testing and prevention for sexually transmitted infections (STIs), birth control, abortion services and preventive screenings such as mammograms.
Alongside physical well-being, reproductive health also includes mental and social wellness. Poverty impacts all aspects of health, but what, specifically, is its influence on reproductive care, and how do economic barriers thwart access?
The role that financial struggles play in access to reproductive health goes beyond whether or not someone is insured, although that's part of it.
"Low-income women, women of color, and non-citizen women are at greater risk of being uninsured," stated the Kaiser Family Foundation (KFF) in its 2021 "Women's Health Insurance Coverage" report. According to Planned Parenthood, 1 in 5 reproductive-age women uses Medicaid to access care.
Even with insurance, low-income women, especially in impoverished rural and urban areas, may struggle with provider shortages, mistrust or prior trauma from the medical system.
How does poverty thwart reproductive care access?
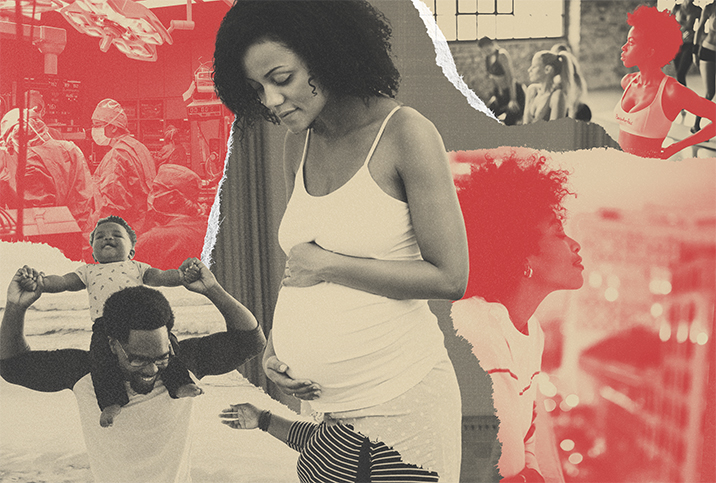
The effects of being low-income compound every portion of reproductive care. Many factors influence showing up to a routine appointment. Finding and affording childcare, access to transportation and being allowed to take time off work all affect a woman's ability to simply get to the waiting room of an OB-GYN office.
But other, more systemic issues impact care, too. Catherine Romanos, M.D., of Reproductive Health Access Project, said pinpointing just one aspect of reproductive care that poverty impacts is a trick question because it's complex—every factor influences the next.
"If you have been historically excluded or maltreated by the medical system, then maintaining any kind of health status is going to be really hard," she said.
Michael Belmonte, M.D., an OB-GYN and Fellow with Physicians for Reproductive Health, said factors such as "speaking a language other than English, cultural differences, geographic location, as well as systemic racism within our healthcare system, also act to further marginalize people."
So, it's more complicated than just poverty impacting a woman's ability to get to a routine appointment. To understand economic access barriers, we need to also examine significant overarching contributors, including how institutionalized racism compounds access.
The impacts of poverty on reproductive issues
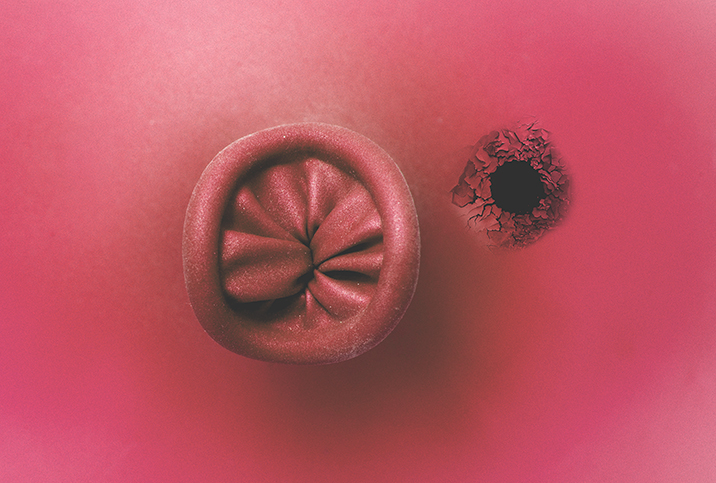
Routine care and preventive screenings, such as Pap smears for cervical cancer and mammograms for breast cancer, are imperative for reproductive health and wellness, and symptoms of underlying medical issues might be missed when routine care is delayed.
"There are many different areas of reproductive health that are affected and, when ignored, lead to worsening of medical issues and make these problems harder to treat throughout a person's life," Belmonte said. "But access to affordable healthcare for all is one way to help shift this disparity.
"People wouldn't feel like they need to wait for problems to become emergencies before seeking care," he continued, "but rather could get routine preventive care and keep people healthy."
'When people don't have access to routine gynecologic care, they must delay pelvic exams and Pap smears, breast exams and mammograms.'
Belmonte added that the disparity in being low-income can impact and intensify multiple forms of care. "When people don't have access to routine gynecologic care, they must delay pelvic exams and Pap smears, breast exams and mammograms."
Delaying routine care could lead to ignoring or putting off atypical symptoms, such as "abnormal bleeding, discharge and pain," Belmonte said. "All these symptoms could be signs of more worrisome things, such as cervical, uterine and ovarian cancers."
In 2018, the Centers for Disease Control and Prevention (CDC) examined cancer rates in counties of Ohio and found higher rates of cervical cancer in the poorest areas. Cervical cancer is largely preventable with screening and vaccines, but you might miss warning signs if care is delayed.
Other atypical symptoms might include menstrual irregularities, which Belmonte said "could be a sign of polycystic ovarian syndrome (PCOS), which can put people at risk for other medical conditions, like infertility or diabetes."
The far-reaching effects of lack of access
What makes access to reproductive care a challenge for low-income communities?
In 2019, KFF sought to examine how being low-income prevents access to reproductive care by holding focus groups in five urban and rural communities in the United States. Rather than looking at statistics, researchers asked community members to inform them on the complicated reasons why reproductive care is difficult to access.
KFF interviewed clinicians, organizers and advocates who work in a range of reproductive and sexual health fields in these locations, along with other members of the communities.
The study revealed similar findings in each community: Poverty and cultural factors impacted the ability to prioritize, afford and obtain family planning or abortion. For states that did not adopt the Affordable Care Act's medical expansion, basic healthcare coverage was a challenge. Provider shortages (specifically providers with language translation services), lack of comprehensive sex ed and abortion services were difficult to access.
Poverty and cultural factors impacted the ability to prioritize, afford and obtain family planning or abortion.
Additionally, the researchers found all of the communities included in the study had a high infant mortality rate. "We see higher maternal mortality, higher prenatal or higher infant mortality" in underserved populations, Romanos confirmed.
In the rural communities, there was an uptick in hospital closures that provided obstetric care. In Selma, Alabama, for example, there was only one maternity ward at the time of the study for the entire seven-county region.
Lack of geographic access to care explains challenges in getting to appointments, which Belmonte said, "has risks to not only the pregnancy, but can have implications that affect the rest of a person's life, like risk of high blood pressure, blood clots and stroke."
A 2020 study by the Commonwealth Fund found that U.S. maternal mortality rates are on the rise. The U.S. has the highest maternal mortality rates among developed countries and lists a shortage in maternity care providers relative to births as a chief reason.
A shift in this disparity
If affordable healthcare is only part of shifting the disparity in accessing reproductive care, what else might help?
"It is important to train a diverse set of healthcare professionals, who are from different backgrounds, speak different languages and connect with different cultures, who have undergraduate training in fields outside of traditional sciences, and many other factors that allow providers to bring their own experiences of the world that allow them to relate to different patients," Belmonte said.
In Selma, Alabama, participants in the KFF research study noted mistrust of the medical community and a shortage of clinicians of color as reasons for difficulty obtaining care.
To shift the disparity, Romanos noted, "We need more people who are from historically excluded communities to be part of the medical system, from hospital CEOs, to doctors and nurses. Everyone needs to see themselves."