Insurance May Not Cover Supplemental Breast Cancer Screening
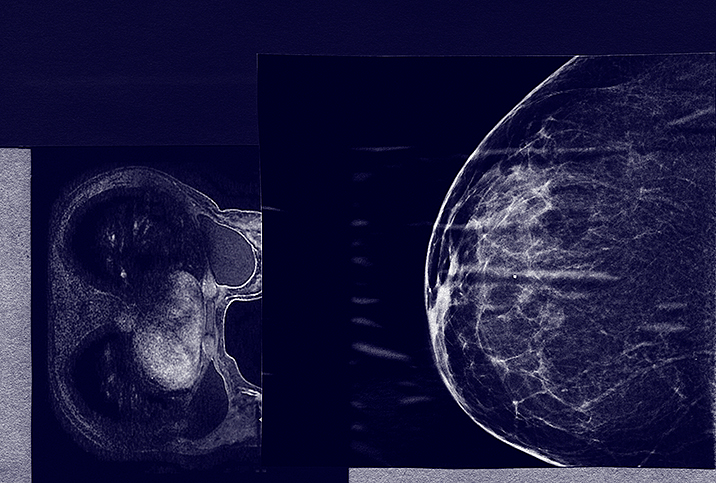
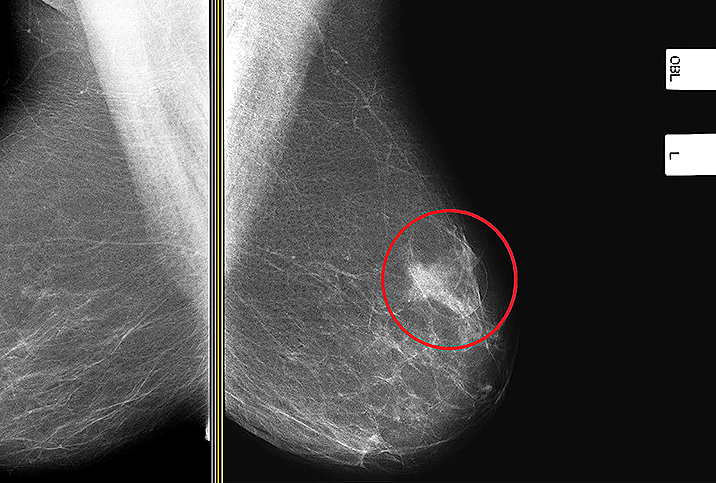
Yearly mammograms may be just the first step in preventive care for those at risk for breast cancer. For people with dense breast tissue, cancer can be difficult to detect with a traditional mammogram, and additional screening may also be recommended.
But who needs additional screening—and how much it will cost—can be difficult for patients to understand, keeping some people from having a screening that could detect cancer earlier, when it is more survivable.
The Affordable Care Act requires that insurance carriers cover the full cost of a screening mammography for women older than 40. But coverage of supplemental screening after the initial mammogram varies, depending on the policy and state.
Even when insurance covers a procedure, it's not always cost-free for the patient. One August 2021 study published on JAMA Network Open found that additional breast imaging exams or procedures occur after 16 percent of initial screenings for insured women 40 to 60 years old.
Coverage for that supplemental screening may include out-of-pocket costs, depending on copays and deductibles. People who get biopsies tend to have greater out-of-pocket costs.
"Having a free first test, knowing that you can't afford any additional care if it becomes positive, it's cruel," said Ruth Carlos, assistant chair for clinical research at the University of Michigan and co-author of the study.
Legislation that mandates insurance coverage for supplemental screening was associated with 6 percent lower odds of cancer being diagnosed at the regional stage.
Insurance is more likely to cover supplemental screening for those who have a high risk of breast cancer. "Most insurance will cover ultrasound for women with dense breasts or MRI screening for women at high risk if requested by a woman's physician," wrote JoAnn Pushkin, executive director of DenseBreast-info.org, in an email.
Pushkin said that MRI is one of the most sensitive tests available, regardless of breast density. It's generally covered by insurance if a person has an estimated lifetime risk of breast cancer greater than 20 percent as calculated by risk models. Having dense breasts is one factor that increases the risk of breast cancer, along with disease-causing gene mutations such as BRCA1/2, a personal history of breast cancer and radiation therapy, and other factors.
An added complication is that some people may not know they have dense breasts, and may not realize they could need additional screening beyond a mammogram to find cancer.
As of June 2021, 38 states and the District of Columbia require a patient be notified of dense breasts after a mammogram—but some states only require that a patient be generally informed of dense breasts, not that they specifically have dense breasts. Only 11 states and the District of Columbia require insurance coverage for supplemental screening after an initial mammogram, according to DenseBreast-info.org.
A study published in August 2021 by the American Journal of Preventive Medicine indicated that the impact of mandated notification of dense breasts alone didn't make a big difference in finding cancer sooner, but that mandates for insurance coverage did.
Legislation that mandates insurance coverage for supplemental screening was associated with 6 percent lower odds of cancer being diagnosed at the regional stage—meaning that cancer is more likely to be found sooner when insurance covers supplemental screening.
Even if patients know they have dense breasts and may need additional screening to find cancer, the cost of tests could keep them from getting the care they need.
"We survey the patients about what are your concerns when it comes to dense breasts, and almost all patients talk about the cost aspect," said Chan Shen, associate professor in the Department of Surgery at Penn State and author of the study. "They say it differently. Person A says, 'Oh, I'm worried about insurance coverage.' Person B says, 'I'm worried about whether I will be eligible for insurance.' Person C says, 'I'm worried about the out-of-pocket costs.'"
Some of the biggest barriers to getting care are the actual cost of care and the perceived cost, which aren't always the same, Carlos said. Even for those who are insured, finding out how much testing will cost can be murky.
A 2017 study Carlos co-authored found that many state and federal insurance plans wouldn't give information on what screenings they covered, or what they did cover didn't follow ACA guidelines.
'Having a free first test, knowing that you can't afford any additional care if it becomes positive, it's cruel.'
This makes it difficult for people to choose the right insurance for them if supplemental screening is important to them. And if people are unclear on what is covered by insurance, their fear of high costs of care may keep them from getting crucial preventive care, even if the actual cost is low.
"We talk about physical symptoms as an adverse event of care—well, I think financial toxicity is just as much an adverse event of care as vomiting after chemotherapy," Carlos said.
While the cost of supplemental screening is a big barrier for patients—and these studies show how much of an impact it can make—Shen said it is just one step in improving care. Additional barriers to care include getting time off to go to appointments, transportation, and general literacy about healthcare. And all people may not have the same issues, or need the same kind of help.
"Legislation in general, whether it's state level or federal level, cannot be the cure-all," Shen said. "There's just not one solution that can solve all the problems."
What does seem clear is that transparency around healthcare costs and insurance coverage can benefit patients who need additional breast cancer screenings. Because, as Carlos said, sometimes what drives a person to get care is about what gets paid for.