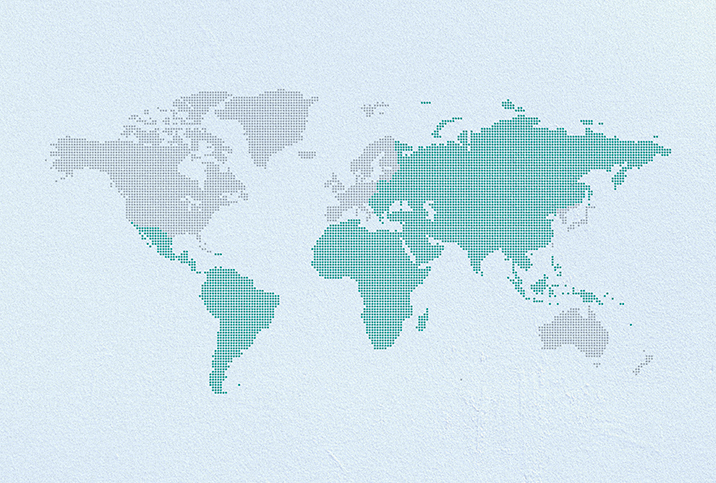
Global Disparities in Cervical Cancer Rates
Cervical cancer occurs in the cells of a woman's cervix, a hollow cylinder connecting the uterus to the vagina. Cervical cancer is nearly always caused by the human papillomavirus (HPV), an infection spread by having vaginal, anal or oral sex, and can be prevented by an HPV vaccination. It is curable if detected and treated early.
The World Health Organization (WHO) has launched an initiative to increase the screening, prevention and treatment of cervical cancer in hopes of eliminating it as a public health issue. Nineteen out of the 20 countries in the world with the highest rates of cervical cancer are in sub-Saharan Africa, including Eswatini, Malawi, Zimbabwe, Zambia, Tanzania and Uganda, according to the World Cancer Research Fund. The key reason for the prevalence of cervical cancer in this region is the lack of access to the HPV vaccine and Pap smears, a screening test that identifies cancerous cells in the cervix.
Risk factors for cervical cancer
Cervical cancer is almost entirely preventable because almost all cases are due to HPV—unlike many other cancers that are caused by an array of physical, hereditary, environmental and lifestyle factors.
There are, however, some common risk factors that increase a woman's chance of developing cervical cancer:
Smoking
Female smokers are roughly two times as likely as nonsmokers to develop cervical cancer. Scientists believe that the byproducts of tobacco damage the DNA in cervix cells and may lead to the growth of cervical cancer. Furthermore, smoking weakens the immune system, making it less effective in combating HPV infections. Cigarette smoke contains cancer-causing chemicals that affect organs beyond the lungs. These substances are carried in the bloodstream throughout the body.
Herpes
Women with genital herpes have a greater risk of getting cervical cancer.
Age
Cervical cancer usually develops some 15 to 20 years after exposure to HPV. This means that most of the women afflicted are in their 30s, 40s and 50s. Women who are 30 and older need to have regular cervical cancer screenings, including a Pap test and HPV test.
Weak immune system
The immune system is needed to destroy cancer cells and slow their growth. Women who have HIV (human immunodeficiency virus), which interferes with the body's ability to fight HPV infections, may develop cervical cancer faster. Taking medications to suppress their immune response also puts them at a greater risk of developing cervical cancer.
HIV
Women with HIV who get infected with HPV are more likely to develop precancerous tissue that can advance to invasive cervical cancer if left untreated.
The WHO recommends cervical cancer screening for all women between the ages of 30 and 49 to identify precancerous and cancerous tissue. HPV vaccination is vital but does not replace the need for screening and early treatment. It's important that women in this age group are screened, whether or not they have had the HPV vaccine, and treated if the precancerous lesion is identified. The higher prevalence of cervical cancer in some regions of the world versus others is largely due to the lack of screening and treatment programs.
Screening guidelines differ across medical organizations, so be sure to consult your doctor about what's best for you based on your age, health and risk factors.