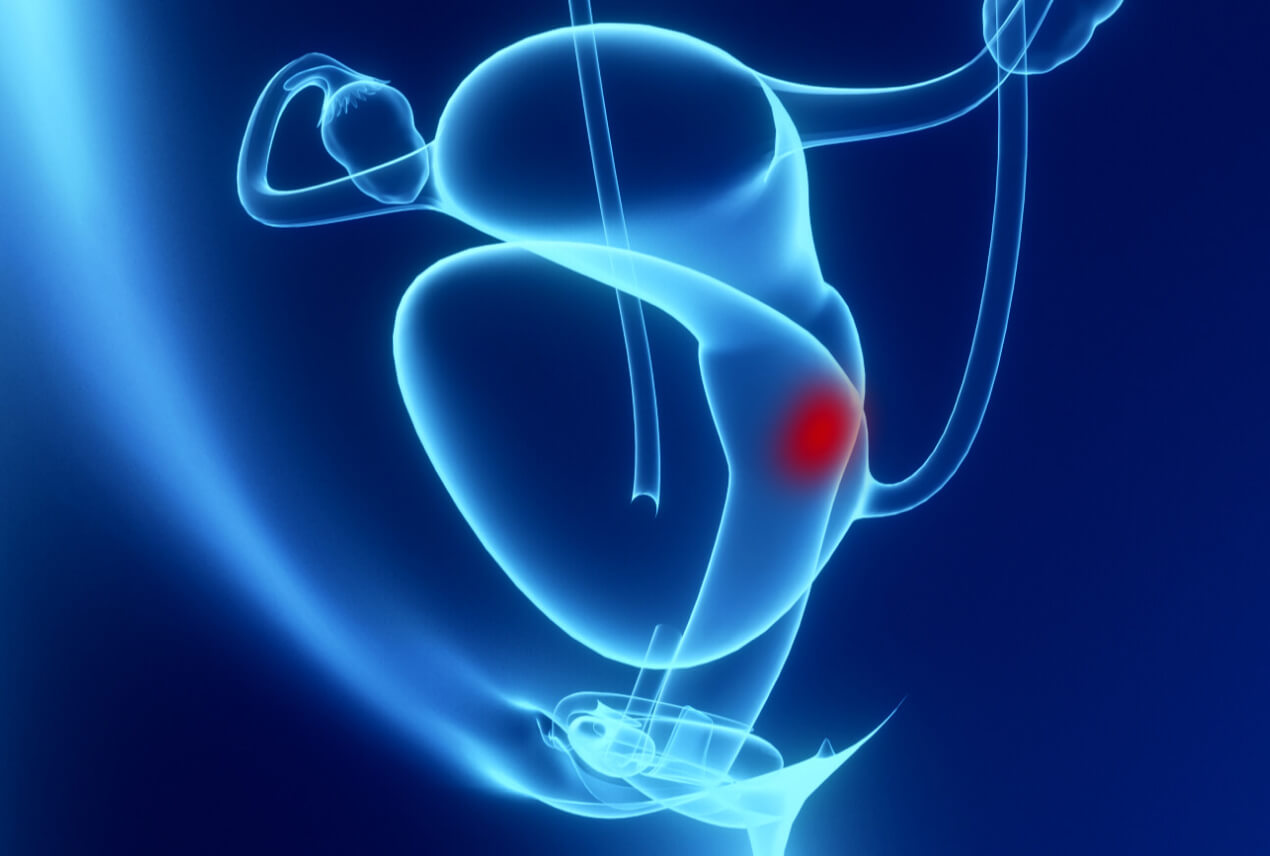
Cervical cancer is easily preventable with regular Pap tests. What are the signs of cervical cancer, who does it affect and what are the treatment options?
It is the fourth most frequently diagnosed cancer among women, according to the World Health Organization (WHO), with 640,000 new diagnoses and around 342,000 deaths globally in 2020.