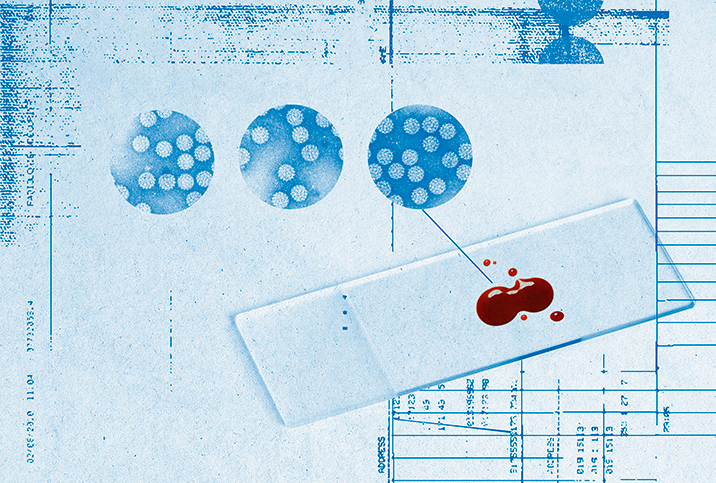
Cervical Cancer: Myths & Misconceptions

Cervical cancer is the fourth most common cancer among women around the world, but it still isn’t well understood by many women. Misconceptions about cervical cancer can leave many women confused and misinformed about its symptoms, prevalence and detection, possibly increasing their risk for disease.
Here are some common myths surrounding cervical cancer, and the reality that debunks them, to help you stay informed about this widespread condition.
Myth: Cervical cancer cannot be prevented.
Reality: Some women believe cervical cancer cannot be prevented, so they avoid visiting their doctor for routine screenings, thinking it will make no difference to the outcome. However, the Centers for Disease Control and Prevention (CDC) reports that up to 93 percent of cervical cancers could be prevented by regular Pap smears and the HPV (human papillomavirus) vaccination. Any cell abnormalities detected in the cervix early can be treated immediately, before they develop into cervical cancer.
Myth: No symptoms means no cervical cancer.
Reality: Early-stage cervical cancer generally produces no signs or symptoms, which means you can have cervical cancer and not know it for several months, or years. Advanced-stage cervical cancer is characterized by symptoms that include abnormal vaginal bleeding between periods and after sex, pain during intercourse, and vaginal discharge with a foul odor that may be heavy, watery or bloody. The best way to determine whether or not you have cervical cancer is to undergo routine screenings, even if you don’t have symptoms.
Myth: A family history of cervical cancer increases my risk.
Reality: Unlike other cancers, a family history of cervical cancer, or a lack thereof, does not affect your chances of developing this disease. The main cause of cervical cancer is HPV, which is often acquired by having multiple sexual partners and engaging in unsafe sex with someone infected by HPV. Other risk factors for cervical cancer include smoking, or having a weakened immune system.
Myth: Cervical cancer affects only older women.
Reality: Cervical cancer is more common among women between the ages of 35 and 44 than in any other age group, but it can still affect women under the age of 20. Given how the primary cause of cervical cancer is HPV, women of any age can be affected by this disease, especially those who meet HPV risk factors such as having multiple sexual partners and having sex at an early age. If you are younger than age 20 and sexually active, ask your doctor about when you should start being screened for cervical cancer. The American Cancer Society recommends that women undergo cervical cancer screening with an HPV test every five years, from age 25 to age 65. These recommendations can be altered, however, depending on high-risk behavior.
Myth: Cervical cancer cannot be treated.
Reality: Cervical cancer can be effectively treated when caught early, which is why routine screenings are important. Early-stage cervical cancer is typically treated using surgery to remove cancer cells and/or the cervix, while radiation therapy or chemotherapy may be used to treat more advanced cases. Immunotherapy and targeted therapy are newer treatments that may also be used to treat cervical cancer.
Ask your doctor for more information about cervical cancer screenings, and about how often you should receive them based on your age and medical history. Your doctor can also debunk any other misconceptions you may have about cervical cancer and work with you to reduce your risk.