Menstrual Blood Shows Promise as HPV Screening Tool
The most common sexually transmitted infection in the United States is genital human papillomavirus (HPV). Left unnoticed and untreated, it can turn normal cells into abnormal cells, potentially leading to cervical cancer.
The Centers for Disease Control and Prevention (CDC) state that 10 percent of women with HPV on their cervix develop long-lasting HPV infections, putting them at risk for cervical cancer. Nearly all cervical cancers are caused by long-lasting infections with high-risk types of HPV.
Clinicians can use screening tests to check for HPV and cervical cell changes caused by HPV. However, the National Cancer Institute recently advised that the number of American women overdue for cervical cancer screening has grown in recent years.
Reasons cited for women not attending cervical cancer screenings include lack of knowledge about screening, not knowing they need screening, lack of access, not having any concerns, living in rural areas and lack of insurance.
A 2018 survey conducted by Jo's Cervical Cancer Trust that included over 2,000 British women found one-third of the respondents were too embarrassed to undergo regular Pap tests. This was due to concerns about their body shape, the appearance of the vulva or concerns over the perceived odor.
For some women, the procedure of cervical screening is too invasive, uncomfortable or off-putting; for others, they simply don't have the time or ability to get to their healthcare provider.
With these factors in mind, a team of researchers set out to investigate if self-collecting menstrual blood at home could be a viable option for diagnosing HPV. Leading the study was Sara Naseri, M.D., the CEO and co-founder of QVin, a women's healthcare service in Menlo Park, California.
Also on the research team was Paul Blumenthal, M.D., M.P.H., professor emeritus of obstetrics and gynecology at Stanford University in Palo Alto, California. We spoke with him to find out more about this promising trial.
Why menstrual blood?
Blumenthal explained that the idea behind the study came from wondering whether menstrual blood could be helpful in testing for various analytes.
"And the bottom line is it turns out menstrual blood is—wait for it—blood," Blumenthal said.
"The correlation between menstrual blood and serum is pretty accurate, and so we became very enthusiastic about this prospect," he added.
The team then looked at what screenings women may need on a semi-regular basis.
"We know women may not want to send blood every month, although there are some things this could be useful for, but in the case of cervical cancer, screening for HPV is useful to do periodically," Blumenthal stated.
The testing process
QVin developed a "Q-pad," a modified menstrual pad that has a removable testing strip. The clinical trial evaluated the concordance between three types of HPV samples: a sample collected with a swab speculum by a clinician, a self-collected vaginal swab and a Q-pad sample for use during the next menstrual cycle. The study included 150 women who presented either for HPV screening or had an HPV-positive history.
"[The Q-pad] is what we would call passive collection," Blumenthal explained. "The specimen comes to you and the blood flows out onto the pad. There is a little tab in the pad that you pull out, which reveals a test strip."
This test strip is then sent to a lab for analysis. It's a dried blood spot so it is not considered hazardous material and does not need a special container. You can simply send it through the mail.
Around 25 percent of patients were uncomfortable with self-swabbing and did not provide a vaginal swab.
How accurate was the testing?
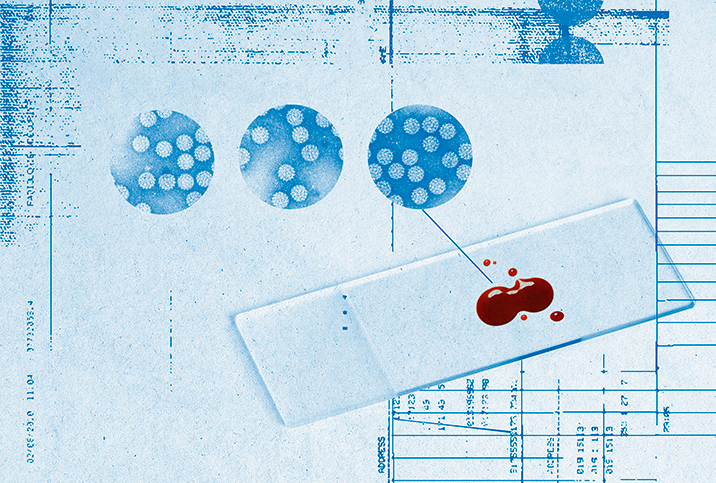
When the self-collected Q-pad samples were compared with the clinician-collected samples, there was a 94 percent to 100 percent rate of agreement in diagnosis, Naseri reported during her presentation at the 2022 annual meeting of the American College for Obstetricians and Gynecologists (ACOG) in San Diego.
This is a very good correlation between samples, said Monte Swarup, M.D., the founder of HPD Rx, a health supplement company in Santa Monica, California, and a board-certified OB-GYN who was not involved in the research but analyzed the study results.
When comparing the samples, the pad correlated highly with those where the clinician-collected swab was positive for HPV. The menstrual pad specimen was positive about 94 percent of the time.
"We think it's very good, especially since this is the first time we've ever really done this," Blumenthal stated, adding the test may not be quite optimized yet.
Among a smaller population of women in the study who had HPV and high-grade precancer, the correlation between the menstrual strip and the clinician-collected swab was 100 percent. Precancer isn't cancer but needs to be treated so it doesn't become cancer.
"So among the women who you really want to identify, we were able to identify all of them," Blumenthal stated.
When comparing the clinician swabs with self-swabs, the correlation between the positive results was about 88 percent.
"So self-swabbing was a little lower than the Q-pad," Blumenthal said. It's thought that women self-swabbing at home were perhaps not always swabbing close enough to the cervix, which lowered the accuracy of the results.
Blumenthal mentioned another interesting element of the study. About 10 percent of women who were positive for HPV on the Q-pad were negative on the clinician-collected swab.
"There could be a few explanations for this, but we think in these cases, HPV was residing higher up in the cervix where the clinician's swab perhaps didn't reach. Whereas with the Q-pad, we know the blood is flowing through the cervix and touching it, reaching those higher areas," he said.
Not just HPV
When looking at other uses for home menstrual blood testing, Blumenthal explained that it could be used the same way as a normal blood test.
A hypothetical example: If you're diagnosed with diabetes, then your HbA1C (blood sugar level) is very high. HbA1C relates to long-term glucose control. But once diagnosed and started on an oral hypoglycemic or insulin, you would want to know the short-term effect of the treatment and if your HbA1C is improving. The Q-pad could be used on a monthly basis to send a blood sample to your healthcare provider without having to take a trip to the doctor's office.
"Almost anything for which you can do an analysis using polymerase chain reaction [PCR], you can probably use the dried blood spot for," Blumenthal said
The biggest benefits of the Q-pad are that it's noninvasive and allows a person to test their blood from home. These features overcome many of the common barriers to screening, such as body concerns, living in a rural area and having to take time off work to attend a doctor's appointment in person.
What are the next steps for this research?
Right now, the Q-pad is still in the testing stage. The next phase for this research would be to do larger studies, Swarup said.
Blumenthal stated that further studies are already happening. A more extensive study looking at HPV involves multiple centers around the United States to get a larger and more diverse group of patients.
Other steps following further research would be looking for regulatory approval from the Food and Drug Administration (FDA).
Using menstrual blood as a diagnostic tool is poised to be a valuable contribution to lifesaving health screenings, and Blumenthal stated it could also destigmatize the menstrual cycle.
"I think, finally, it's probably important to recognize that this isn't really a new test," Blumenthal said. "This is the same HPV test that we're going to do no matter what the source. It's just a different and innovative collection system."