Getting a Colposcopy: What to Know and How to Prepare

Getting a yearly Pap smear may seem routine to most women, and if the results come back clear, you likely don't think much about these visits. But if your Pap smear ever comes back abnormal, you may receive a call to go back in to see your doctor. At that point, the gynecologist may decide to review your Pap again after a certain period of time, redo the exam or, in some cases, order a colposcopy.
What is a colposcopy?
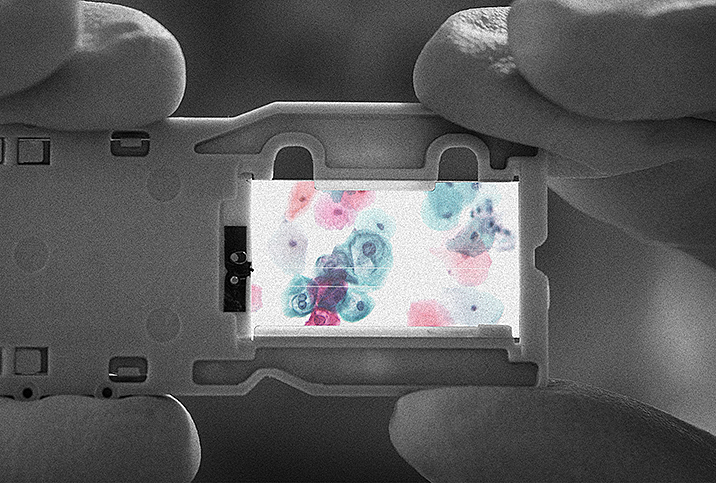
A colposcopy is performed to check your cervix for anomalies if your Pap smear results come back abnormal. During this procedure, your OB-GYN will use a colposcope—a medical tool with a magnifying lens—to check your cervix, the opening of your uterus and your vagina for abnormalities.
The procedure typically lasts between five and 10 minutes, and is usually performed in one of your gynecologist's exam rooms.
Why is a colposcopy performed?
If you have an abnormal Pap test, a colposcopy allows your doctor a closer look at your cervix to see if anything more serious is going on. A colposcopy can diagnose a variety of issues, such as:
- Genital warts
- Cervicitis (inflammation in the cervix)
- Precancerous cervical tissue
- Precancerous vaginal tissue
- Precancerous cells in the vulva
What to expect during a colposcopy
For some women, getting a colposcopy will feel similar to a Pap smear, but the pressure might be slightly more intense. Your gynecologist will use a speculum to hold your vagina open and then dab a vinegar solution onto your cervix. The doctor will then view your cervix with the colposcope.
The vinegar solution might sting slightly, but it's extremely important because it plays a key role in allowing your doctor to see if there are any abnormal spots on your cervix. Any precancerous or cancerous cells on the cervix will absorb more of the vinegar, making them look whiter than normal tissue. This directs the doctor to where to do the biopsies.
In some cases, depending on your previous Pap results, medical history and whether or not abnormalities are present, the doctor will perform a cervical biopsy. This means that during the colposcopy, your doctor may collect tissue samples of your cervix. If a biopsy is needed, you'll likely experience minor pain and discomfort during the tissue removal, but thankfully, the process typically lasts only a matter of seconds. The tissue samples would then be examined at a lab.
You will likely experience light bleeding after a biopsy, and may have cramping and pain for a few days. Prolonged cramping and pain, however, is extremely unlikely.
Preparing for a colposcopy
Getting ready for a colposcopy is pretty easy, but there are a few tips you might want to keep in mind to avoid issues and minimize discomfort:
- Don't schedule your procedure during your period.
- Refrain from sexual intercourse and tampon use for 48 hours before your procedure.
- Don't use vaginal medications 48 hours before your procedure.
- Consider taking ibuprofen or acetaminophen just before your procedure.
After your colposcopy
Once the procedure is over, be sure to ask your doctor when you'll find out the results. You should always know the results of any biopsy, whether it is normal or not, so ask about their office policy.
The results of your colposcopy will determine your next steps. Many women simply have monitored Pap smears for a few years after, while others may need further testing. Be sure to ask your doctor any questions you might have about your results.