3 Unique Causes of Genital Pain to Avoid at All Costs
Most guys know the sensation of getting hit in the testicles. To describe it as an unpleasant experience would be a massive understatement. While it's easy to say, "Don't let anyone hit you below the belt," avoiding genital pain isn't always that simple.
Sometimes, a man may sit down the wrong way or do something damaging to their genitals while tossing and turning in their sleep. Other times, intercourse can lead to a painful situation.
Those are unfortunate occurrences. But some lesser-known medical causes of genital pain can also be agonizing, and it would be best to avoid them entirely if possible.
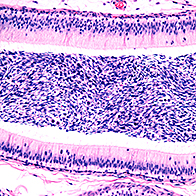
Chronic pelvic pain syndrome (CPPS)
Enduring pain, especially without explanation, can be discouraging. Few experiences match it, and chronic pelvic pain syndrome (CPPS) falls into that category.
"Sadly, millions of men live with chronic pelvic pain syndrome," said Dan Sperling, M.D., founder of the Sperling Prostate Center in Delray Beach, Florida. "No one has yet found the exact origin of the pain, though it is often attributed to chronic prostatitis, even when no infection or inflammation can be diagnosed in the prostate."
CPPS is a strange condition in that it doesn't have a single, discernible cause. Many urologists consider it to be an amalgamation of several underlying factors, and as a result, treatment typically involves several different methods, depending on the severity of the condition and its main problematic effects.
"Pelvic floor dysfunction, which was once more commonly associated with females, is now a growing field in men," said Aram Loeb, M.D., of the University Hospitals Urology Institute in Cleveland. "Men are often treated numerous times with antibiotics only to have the symptoms return. This can be extremely frustrating and demoralizing for men as they get passed around to different physicians with no resolution of their pain."
Sperling said many cases of CPPS seem to be caused by tension in the muscles of the pelvic floor.
"These muscles, along with nerves and ligaments, form a sling that supports the reproductive organs, urinary tract and digestive tract within the pelvic area," he said. "Once pain begins, it can actually lead to more tension and increased pain."
The increased pain signals being sent to the brain can also alter a person's biochemistry over time.
A 2016 study on CPPS in men suggested urologists encourage patients to engage in as many activities of daily life as possible. Unfortunately, this chronic pain is so intense, it can interrupt many aspects of daily life and take a psychological toll alongside the physiological toll on the patient.
Despite the obstacles, a good treatment plan can make CPPS more bearable.
"After a referral to a male pelvic floor physical therapist, a patient will receive an initial assessment, and based on that, a treatment plan will be initiated to restore normal function through manual therapy, relaxation, and strengthening and coordination exercises," Loeb said. "There is much success when men commit to seeing a PFPT and actively participate in their treatment plan."
Urethral stricture
It's common to hear about urinary tract infections (UTIs) and how painful they are, but they aren't the only potential issue that can affect the urethra. Urethral stricture refers to scarring in the urethra that creates a narrowing or blockage that restricts the flow of urine. Think of it as a clogged drain when you have low water pressure, except you can't use Drano to clear it.
"Symptoms include urinary problems—such as difficulty starting, a weak flow, frequent sense of urgency, pain when urinating, blood in your urine—and consistent bone pain, especially in the pelvis and lower back," Sperling said.
Many of these symptoms overlap with those of prostate cancer, and, in fact, urethral stricture can result from prostate cancer. Other causes of urethral stricture include damage to the pelvic region, long-term catheter use, prostate surgery, sexually transmitted infections (STIs) and radiation therapy.
Treatment methods include dilation, or enlarging the stricture with gradual stretching; urethrotomy, which involves cutting the stricture through a scope with a laser or knife; and open surgery, which is the removal of the stricture with reconstruction of the urethra.
An untreated urethral stricture can lead to problems such as infections, inflammation, stones and, potentially, urinary retention, or the inability to pass urine.
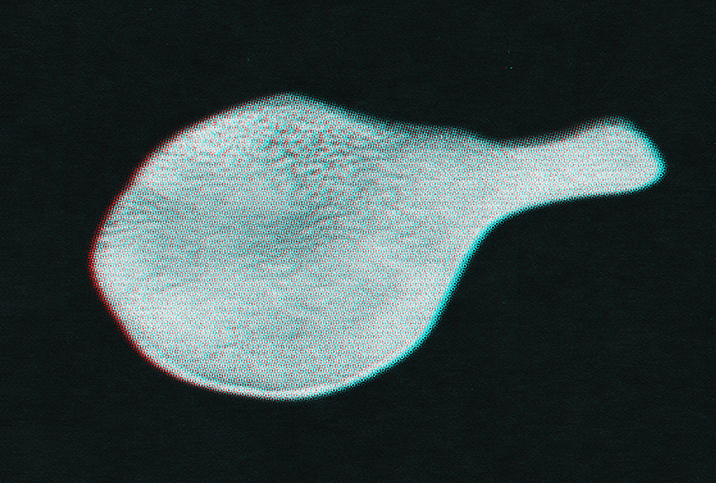
Scrotal swelling
"Ball pain is a common complaint that we see in the office every day," Loeb said. "The typical evaluation involves a consultation where we talk about the onset, duration and severity, as well as alleviating or exacerbating factors, and other associated symptoms."
One issue he sees in patients is the development of a hydrocele, which causes scrotal swelling due to fluid collecting around one or both testicles. Generally, a hydrocele is caused by a weak point in the genital wall that lets in excess fluid, but it can also result from inflammation or injury to the scrotum or, in older men, infections, including STIs.
While a hydrocele is far less painful than many other genital issues—generally, it is more uncomfortable than excruciating—any extra fluid or blood in the scrotum can be a sign of infection, inflammation, kidney stones or cancer, Loeb said.
Loeb identified another cause of scrotal swelling: a varicocele, which is the enlargement of the veins in the scrotum that develops over time. Thankfully, in most cases, a varicocele isn't painful and can be fixed with surgery, but in rare cases, it causes pain and hinders the production and quality of sperm, leading to infertility.
Pain caused by a varicocele varies throughout the day, often worsening with physical exertion or long periods of standing, and generally decreasing during periods of lying down.
Preventing genital pain
Medical professionals say this often, but only because it can't be stressed enough: If you have any pain or abnormal feeling in your genitals, see a doctor. There's nothing tough or "manly" about refusing to seek help, and it's always better to address issues as soon as they arise. Most conditions worsen over time when they're left untreated.
"Men have unique health needs, and we can address them at every stage of their lives," Loeb said. "In Cleveland alone, 250,000 fewer men see a doctor annually compared to women."
Additionally, men can always make some lifestyle changes that benefit sexual health as well as overall health.
"Regular exercise is critical to healthy sexual fitness, including cardiovascular and core strengthening, which are helpful in maintaining the health of the pelvic floor and genital area," Loeb said. "I also think it's important for men to perform routine self-examinations."
Sperling recommends eating a heart-smart diet full of healthy fats and proteins.
These actions can't guarantee you won't experience a painful genital condition at some point in your life, but treating your body well can help it continue to function properly.