Life & Sex after Rectal Cancer

Surgical and therapeutic advances allow rectal cancer patients to live longer. Yet, rectal cancer survivors often overlook and avoid acknowledging any lingering sexual problems—even those patients whose quality of life has been regularly affected by sexual dysfunction and discomfort—according to a study published in the Journal of Gastrointestinal Oncology.
If you think this may be the case for you, assess your symptoms closely and take a look at some available solutions.
Cancer treatment & sexual wellness
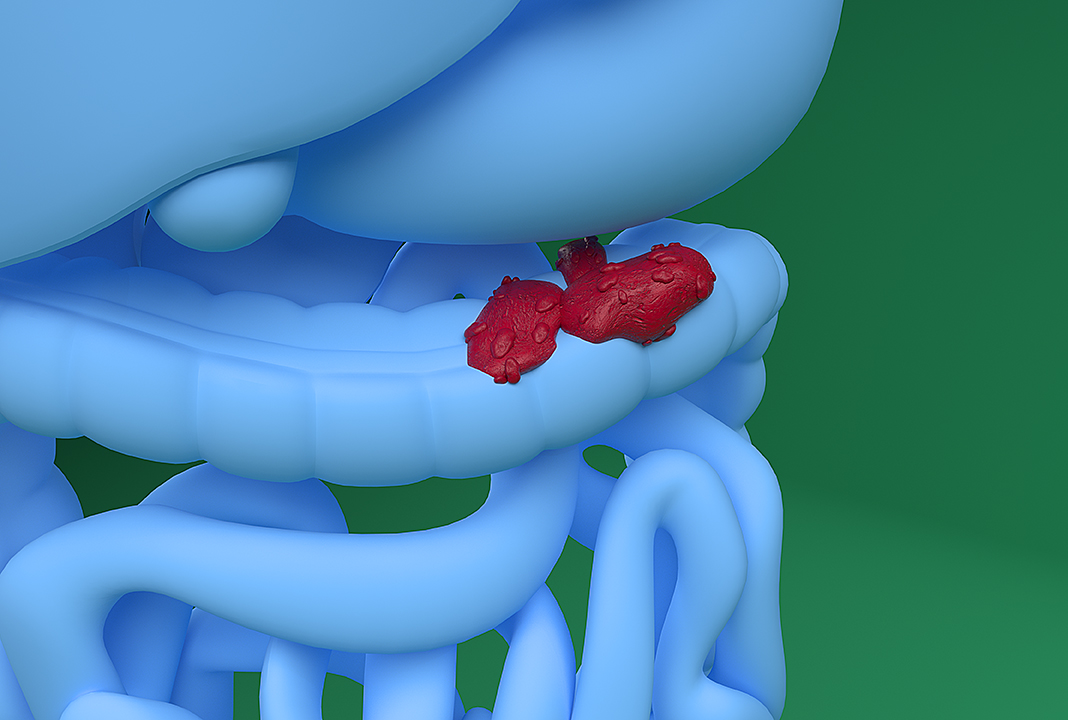
The most common treatment for rectal cancer is surgery, and the type of surgery will depend on what stage the cancer has reached, according to the American Cancer Society (ACS). If the rectal cancer is in an early stage, surgery can usually be performed through local incisions. For more advanced cases, however, major surgery may be required.
For patients in the later stages of rectal cancer, surgery is sometimes carried out through several incisions in the abdomen, and in some cases, parts of the rectum are removed. A patient who has part or all of the rectum removed may end up with a temporary or permanent colostomy or ileostomy. In this case, the colon is redirected to an opening in the skin made in the abdomen and attached to a stoma, where a bag collects stool.
The ACS reports that while surgery is the most common treatment for rectal cancer, it is usually done in conjunction with chemotherapy and radiation therapy. Both of these therapies can negatively affect a person’s sex drive, and research has shown that both men and women tend to experience sexual problems and quality of life issues following rectal surgery.
In addition, having a colostomy can impact an individual’s body image and overall sexual comfort. After rectal surgery, patients may experience abdominal pain during sex and in everyday life.
ED may be a problem
When a person gets rectal surgery that requires abdominal incisions, they can develop scar tissue that makes organs and tissues stick together; this type of scar tissue is known as an adhesion. An adhesion may cause discomfort, because it prevents the normal free sliding of the intestines within the belly. If this is an issue for you, talk to your doctor, because in some cases, further surgery may be necessary to remove the scar tissue.
In men, some types of rectal surgery have been shown to cause erectile dysfunction (ED) and less intense orgasms, which is likely tied to nerve damage from the surgery if it is extensive. Men who undergo a type of rectal surgery called an abdominoperineal resection can also experience fertility issues.
As for women, most rectal surgeries don’t result in loss of sexual function, though adhesions can cause pain or discomfort. However, women in some studies have reported sexual dysfunction. Rectal surgery doesn’t affect a woman’s fertility unless her uterus is removed.
It’s important to talk with your doctor before undergoing rectal surgery to find out how it will affect your body and sex life. Though surgery may be necessary to treat the cancer, discussions with your doctor and loved ones—as well as research online—can help you mentally prepare for what comes next.
Talk about it
Patients often choose to avoid discussing sexual health because it makes them uncomfortable, while overscheduled healthcare professionals may not take the time to ask patients about sexual health as a quality-of-life issue.
In fact, a 2014 study published in Psycho-Oncology noted that 58 percent of cancer survivors surveyed wished their primary care physicians would ask them about their sexual health, while more than 90 percent said oncologists rarely addressed the subject.
Most rectal cancer survivors choose to remain sexually active, but many experience depression, relationship complications and an eroded sense of well-being when problems like discomfort, body image issues, loss of libido and ED are left unaddressed.
Communication between patients and healthcare providers is essential to maintaining a high quality of life. Clinicians can especially help rectal cancer survivors achieve that goal by encouraging them to voice concerns about their sexual dysfunction. But don’t be shy; if they don’t mention it, don’t hesitate to bring up the subject yourself.
Establishing a comfortable forum for communicating problems and candidly discussing solutions can help patients come to terms with any postoperative sexual health problems.