Colorectal Cancer: Myths & Misconceptions
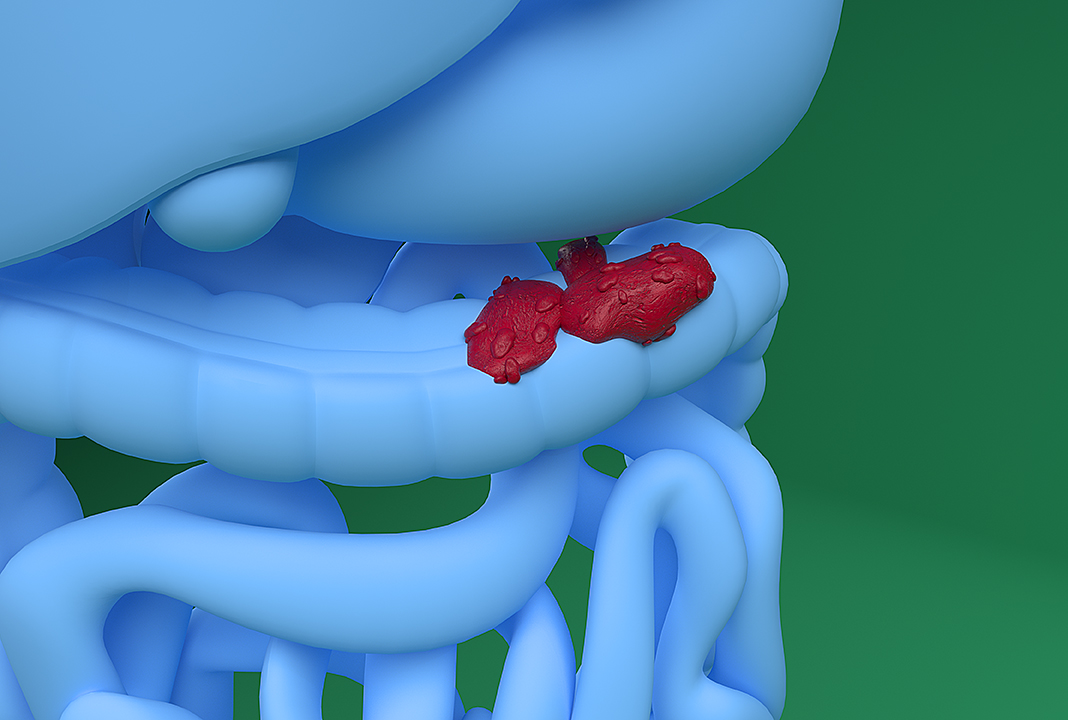
The colon, also known as the large intestine, is part of the body’s digestive system. Approximately 6 feet long, it absorbs water from digested food and, using muscular contractions, pushes stool to the rectum for evacuation.
The inner lining of the large intestine is home to millions of cells that can change and lead to abnormal growths called polyps. Over time, some types of polyps can become cancerous, leading to colorectal cancer.
While colorectal cancer is serious, not everything you hear about it is true. We hunted down five of the most prevalent myths about the condition, and then found the appropriate research to debunk each misconception.
Myth: Colorectal cancer affects only white men.
Reality: Colorectal cancer affects all races and sexes, although African American men and women get colorectal cancer at higher rates than men and women of any other racial or ethnic group in the United States. Men are more likely to get colorectal cancer than women, and it is considered extremely rare in children and young adults under the age of 19.
Myth: Colorectal cancer cannot be prevented.
Reality: Like with most diseases, especially the majority of cancers, lifestyle choices can reduce risks. For example, eating a healthy diet and maintaining physical fitness through consistent exercise can lower a person’s probability of contracting colorectal cancer.
Myth: Young people can’t get colorectal cancer.
Reality: While one’s chances of getting colorectal cancer increase with age, it is still possible for a younger person to get colorectal cancer, though the chances are low: affecting far fewer than 1 person in 100. Research carried out by the National Cancer Institute revealed that only 6 percent of individuals diagnosed with colorectal cancer were younger than 50 years old.
The American Cancer Society encourages people to begin regular cancer screenings at age 45. Research acknowledges that patients with inherited syndromes are even more likely to develop colorectal and other cancers during their youthful years, so knowing your family medical history is important.
Myth: If I don’t have symptoms, I probably don’t have it.
Reality: Actually, it is common for colorectal cancer, in its earliest stages, to present no visible signs at all. As a result, colorectal cancer is often diagnosed in its later stages, when patients develop abdominal pain, rectal bleeding, weight loss, progressive diarrhea and constipation, weakness and fatigue, vomiting, a mucus-like substance in the stool (especially noticeable when wiping), and unusual food cravings. Scheduling regular screenings is important so the disease can be diagnosed early.
Myth: Colonoscopies are uncomfortable and unpleasant.
Reality: Yes, the procedure is uncomfortable for some people, but efforts are made to make it as comfortable as possible. A colonoscopy is a routine outpatient procedure that does not require an overnight stay at the hospital. There is some preparation involved, including drinking medicine to facilitate clearing your bowels the night before. At the start of a colonoscopy, the patient is given a mild sedative to relax, and a flexible tube with a tiny camera in its tip is then inserted into the rectum, allowing the doctor to analyze the inner lining of the large intestine. The process is usually complete within two hours, and the patient is awake and ready to go home without any discomfort.
As a first step, you can take a stool sample yourself and mail it to a lab for analysis. If the lab uncovers evidence of blood in the stool, you’ll be advised to have a follow-up colonoscopy.
The good news is colorectal cancer is curable, but it must be detected in its early, asymptomatic stage. Talk to your doctor and decide on a strategy to start screening early.