Could Epididymitis Treatment Be as Simple as Testicular Stretches?

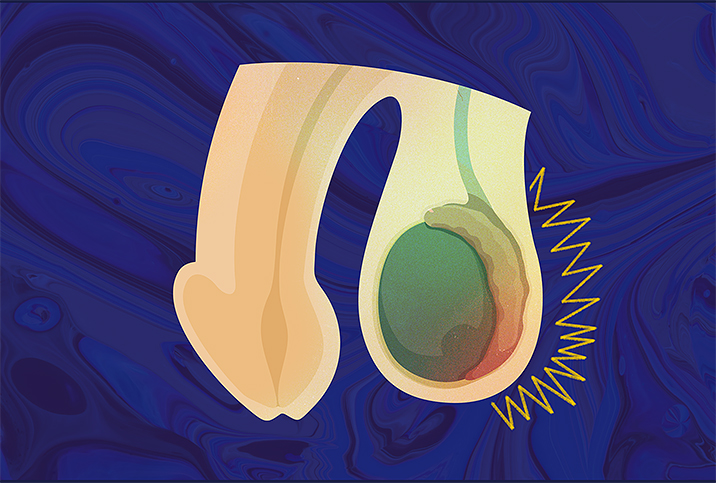
Epididymitis is a common men's health issue, with about 600,000 cases reported in the United States every year. At its simplest, epididymitis occurs when the epididymis becomes irritated or inflamed from an infection.
Treating the infection is simpler when doctors are positive the epididymis is causing the pain or irritation. When the source of discomfort is more difficult to pinpoint, however, treatment becomes more complicated.
When it's clear the epididymis is infected, care is pretty straightforward. However, when the regular course of antibiotics doesn't improve symptoms, the path to relief becomes more experimental and intensive.
What is epididymitis?
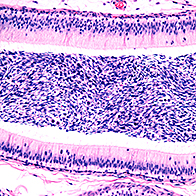
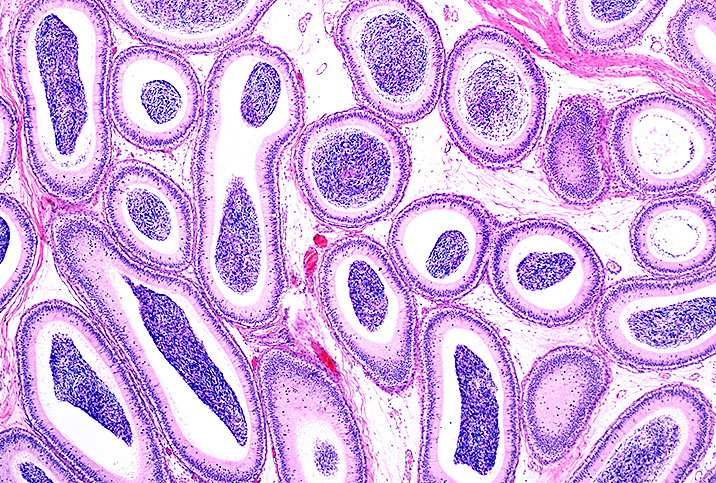
Before learning about epididymitis, it's important to know what the epididymis is. It is a 20-foot-long coiled tube at the back of each testicle where sperm is stored and transported during ejaculation.
A patient's symptoms usually start with pain on one side of the testicle. However, symptoms can also include a frequent need to urinate, a fever or a lump on the testicle.
Epididymitis isn't something to take lightly. If the epididymis is damaged by a bacterial infection, for example, it could cause a blockage of sperm. In rare cases, that could lead to infertility.
What are the risk factors of epididymitis?
The main risk factor for epididymitis is contracting a sexually transmitted infection (STI) through sexual activity, according to Kevin Chu, M.D., a fellowship-trained urologist who specializes in men's health and male fertility and practices in Los Angeles.
"If someone's under 35, we suspect the epididymitis could be secondary to a sexually transmitted disease," Chu said. "So we generally check for chlamydia, gonorrhea and other STIs in the urinalysis test, since these could be causing the epididymitis. For people over the age of 35, we check for E. coli, which is usually found in urinary tract infections."
What are some simple epididymitis treatments?
Epididymitis is generally divided into two types: short-term (acute) and long-term (chronic).
"Epididymitis comes from the swelling of this scrotal area, which can cause pain," Chu explained. "If there's a sudden onset of pain, a urologist first checks to see if you have a urinary infection."
"If you have a urinary infection, the straightforward way to treat it would be to give some antibiotics for approximately one to two weeks. We also try using ice packs and other conservative measures," Chu noted.
Iliopsoas stretches could help resolve chronic testicular pain in some people, suggested a 2021 study. Speak to your doctor to see if stretching the inner muscle of your hip could help you too.
What are the more intensive epididymitis treatments?
The simpler treatments for epididymitis usually work, but there are rare cases where the infection doesn't respond to antibiotics. In those situations, abscesses can form on the epididymis and get worse over time. This is referred to as chronic epididymitis.
"Chronic epididymitis and chronic testicular pain, in general, can be quite difficult and frustrating to treat," said Majdee Islam, M.D., a urologist and men's health specialist at Urology of St. Louis.
This is particularly true, he added, when:
- The antibiotics don't work and the pain continues
- There is no infection found, but the pain continues
- The pain keeps returning despite treatment
In those more complicated cases, doctors attempt to make sure it's the epididymis causing the pain. The investigation often begins with a scrotal ultrasound.
Doctors also check for chronic prostatitis. They conduct a prostate exam or tests to assess the prostatic fluid to see if bacteria are hiding in the prostate gland but not appearing in the urine.
Occasionally, a computed tomography (CT) scan is performed to look for abnormalities that could cause obstruction, such as urine backing up into the epididymis or prostate.
"Sometimes, despite all of this, we cannot find a root cause for the symptoms," Islam said.
In those cases, it's time to turn to other treatment modalities, including some potential alternative therapies.
Chu explained that doctors might try:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) to decrease inflammation in the scrotum
- Neuropathic medications such as gabapentin
- Acupuncture
- Pelvic floor therapy
Acupuncture has been shown to help improve symptoms and relieve the pain associated with epididymitis. It won't, however, cure the ailment.
In chronic cases, treatment becomes a combination of pain management—even if doctors can't get your pain to zero—and figuring out the root cause of the discomfort.
One option is a spermatic cord block, an injection of numbing medication mixed with a steroid into the spermatic cord to decrease discomfort and calm the nerves, Islam said.
The last line of treatment is an epididymectomy, a surgery that removes the epididymis. Doctors may also strip the spermatic cord down to remove the nerves that may be contributing to the pain, or even remove the entire testicle, Islam added.
Surgeons perform an epididymectomy only if urologists determine an inflamed epididymis is the sole cause of pain. There are risks involved with this surgery, but 75 percent to 85 percent of patients experience a resolution of pain.
The success rate is high because of the careful patient selection for the procedure, Chu said.
The sooner it's treated, the better
Invasive treatments such as an epididymectomy are undertaken only if patients don't respond to low-risk options, such as antibiotics or physical therapy. In the rare case that a patient does need surgery, it's an outpatient procedure. Patients can usually return home the same day.
The best way to avoid chronic epididymitis is to not leave it untreated. A general rule of thumb is to see your primary care physician if you start feeling pain on one side of a testicle. This type of pain isn't normal and shouldn't be ignored. Doctors can run a urinalysis and check for an infection, giving you peace of mind and starting treatment if needed.