Marked by inflammation of the prostate, prostatitis can cause pain, discomfort, urinary issues and other symptoms.
The Facts About Prostatitis
Find out how prostatitis affects your sexual health.
What is prostatitis?
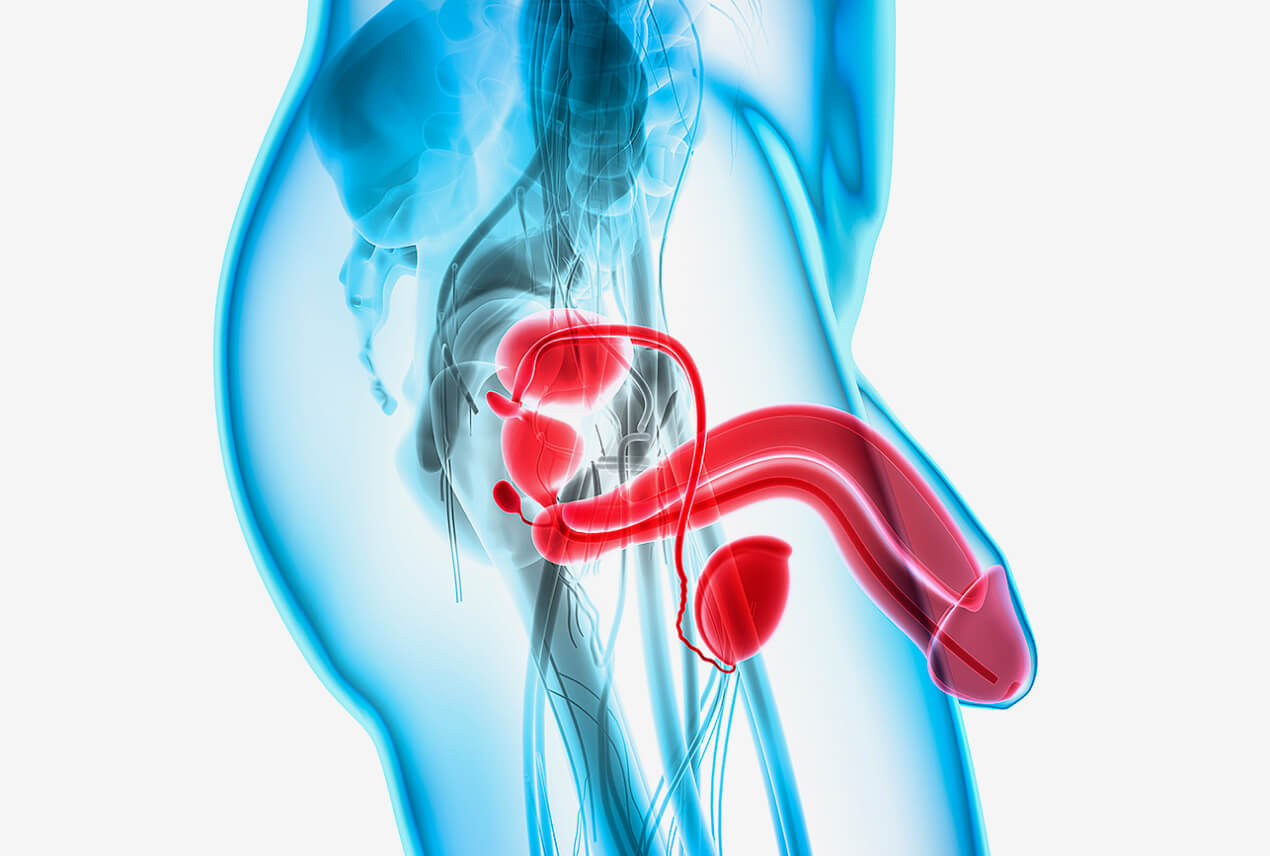
The prostate is a small, walnut-sized gland found only in men (and transgender women). It sits just below the bladder and partially surrounds the bladder neck, the place where the urethra connects to the bladder. In terms of male reproduction and sexuality, the prostate is a crucial player.
Urinary habits experience effects when the prostate isn't healthy.
The prostate gland is responsible for producing seminal fluid, which makes up about 25 percent to 30 percent of a man's ejaculate. One of its major tasks is to pump this fluid into the urethra when the man is about to ejaculate, where it mixes with sperm and other fluids. The seminal fluid helps to protect and nurture the sperm cells to give them the best chance of reaching their destination.
A common dysfunction of the prostate gland is prostatitis, which involves inflammation and swelling.
What are the types of prostatitis?
Prostatitis presents with symptoms of inflammation, irritation and swelling of the prostate gland. While it is related to the prostate gland, it's important to note that prostatitis is not related to prostate cancer.
There are several distinct types of prostatitis, according to Cleveland Clinic, each of which may require a different treatment approach.
Acute bacterial prostatitis
This type of prostatitis occurs when a urinary tract infection (UTI) reaches the prostate gland. It may cause fever and chills and painful and frequent urination, and it requires prompt medical intervention.
Chronic bacterial prostatitis
When bacteria gets trapped in the prostate gland, it can cause recurrent UTIs and chronic prostate discomfort.
Chronic pelvic pain syndrome (CPPS)
The most common type of prostatitis is widely thought to be CPPS. Approximately 1 in 3 men experience prostate gland inflammation, which may present alone or concurrently with chronic pain in other parts of the pelvis, lower back, hips, genitals or perineum—the area between the testicles and the anus.
Asymptomatic inflammatory prostatitis
This is a condition in which the prostate gland is inflamed but you don't experience any symptoms. After being tested for other reasons, such as fertility, your healthcare providers may notice the prostate is inflamed.
If you're not experiencing any symptoms, they'll likely recommend leaving it untreated and suggest a watchful waiting scenario to make sure it doesn't get any worse.
What causes prostatitis?
The four different types of prostatitis highlighted above each has its own causes and risk factors.
The most common type of prostatitis, according to Cleveland Clinic, is CPPS, the causes of which still aren't entirely clear. However, researchers and healthcare providers believe there is evidence pointing to dysfunction in the pelvic floor muscles as one underlying cause.
The entire area is shot through with nerves running from the lower spine to the genitals and other parts of the pelvis. It's believed that autoimmune diseases, stress, pain or tension in one spot can cause referred pain in another, including the prostate gland.
Causes of the two bacterial types of prostatitis include the following:
- Bladder infections
- Bladder stones
- Prostate stones
- Surgery or having a biopsy that uses a catheter
- Urinary retention (not being able to fully empty the bladder)
- UTIs
How common is prostatitis?
Prostatitis is the most common urinary tract problem for men younger than age 50 and the third-most common for men older than 50, according to the U.S. Department of Health and Human Services. About 2 million yearly visits to healthcare providers come as a result of prostatitis in the United States.
Overall, the condition affects 10 percent to 15 percent of the U.S. male population.
Who is at risk for prostatitis?
The risk factors for prostatitis vary, depending on which type we're talking about. When it comes to the bacterial types, much of the risk comes down to how likely it is that a bacterial infection can make its way up the urinary tract and into the prostate gland.
The other major risk factor is being younger than 50.
Some other common risk factors for bacterial forms of prostatitis include the following:
- Having a biopsy taken of the prostate gland
- Having a urinary catheter inserted
- Having an infection of the urinary tract
- Previously having prostatitis
Risk factors for CPPS-related prostatitis include:
- Autoimmune diseases
- Pelvic floor muscle dysfunction
- Stress
Symptoms of prostatitis
The symptoms of prostatitis vary by individual, but the prostate gland's location means these symptoms are often related to the urinary tract and sexual function. They often include the following:
- A weak stream, or a stream that starts and stops when urinating
- Blood in the semen
- Erectile dysfunction (ED)
- Frequent urge to urinate
- Lower back or hip pain
- Pain in the testicles, penis or perineum
- Pain during sex
- Painful ejaculation
- Painful urination
How is prostatitis diagnosed?
Diagnosing prostatitis involves your healthcare provider narrowing down which type of condition you may have since the treatments vary so much. Three of the preliminary, less-invasive types of diagnostic tools they may use include a digital rectal exam (DRE), a urinalysis and a blood test.
Digital rectal exam
The prostate gland's location means that trained healthcare providers can insert a finger into your rectum and, pressing forward on the front wall, deduce what they need to know about your prostate gland without having to cut, insert a scope into your urethra or use expensive equipment.
For instance, they may be able to detect if the prostate gland is enlarged or if there are hard spots on it that may indicate cancer.
Urinalysis
Testing your urine can tell inform your provider if you have a bacterial infection or UTI.
Blood test
A prostate-specific antigen (PSA) test, carried out by a blood draw, can provide information on your prostate's production of this protein. High levels may indicate prostate cancer, prostatitis or benign prostatic hyperplasia (BPH).
If further testing is required, two invasive diagnostic procedures are a cystoscopy and a transrectal ultrasound.
Cystoscopy
This test uses an instrument called a cystoscope. The cystoscope has lenses like a telescope or microscope and is inserted into the urethra to examine the urinary bladder for other urinary tract issues that may be related to prostatitis.
Transrectal ultrasound
Men with chronic bacterial prostatitis that doesn't improve with medication may undergo a transrectal ultrasound. This is a test in which a small, lubricated probe is placed into the rectum and releases soundwaves to create echoes as they enter the prostate to produce images of the prostate gland.
How is prostatitis treated?
Again, it's necessary to break down prostatitis treatment into two separate categories: bacterial types and CPPS types.
For acute bacterial prostatitis, a course of antibiotics will usually clear up the condition. Occasionally, more severe cases may require intravenous antibiotics.
Treating chronic bacterial prostatitis is more difficult and may require up to three months of antibiotics. If that doesn't work, long-term, low-dose antibiotics may be used to prevent future flare-ups.
Treatment for CPPS-related prostatitis can be even more complex. Many providers follow what's called the UPOINT checklist, offering a mix-and-match variety of treatments specific to the following symptoms:
- Infection. Antibiotics are used to kill infectious bacteria.
- Neurologic. Medications such as amitriptyline (Elavil) can help with neurologic pain of the type that results from fibromyalgia or CPPS.
- Organ. Quercetin, a plant flavonol believed to have antioxidant and anti-inflammatory effects, along with bee pollen, may help relieve prostate swelling and inflammation.
- Psychosocial. Stress management, counseling and anxiety medications may help some men.
- Tenderness. Pelvic floor physical therapists can help by teaching men how to release tight muscles.
- Urinary. Medications such as tamulosin (Flomax) can help relax the prostate and release its grip on the urethra, allowing for easier urination.
What are the complications of prostatitis?
Many of the prostatitis complications that men notice right away include problems with sexual functioning, such as:
- Erectile dysfunction. Pain anywhere in the pelvic region can cause problems with getting and maintaining an erection. Also, the psychological trauma of experiencing painful ejaculation may lead to future ED when the next sexual encounter comes along.
- Inflammation of the sexual organs. Inflammation of the prostate gland can cause inflammation of nearby organs, including the penis and testicles.
Other complications may include:
- Bacteremia. This is a bacterial infection of the bloodstream.
- Prostatic abscess. This rare condition occurs when a pus-filled cavity forms in the prostate.
- Urinary retention. A chronically swollen and inflamed prostate gland impinging on the urethra may grow so acute that it prevents urine from being released at all. This is a medical emergency and requires immediate care.
How to prevent prostatitis
No current research demonstrates any reliable way to prevent prostatitis. It's still a relatively poorly understood condition.
However, getting prompt treatment for UTIs and being sure to take the entire course of any antibiotics you're prescribed may help prevent a bacterial infection from spreading to the prostate.
Recognizing if you have pain in your perineum when sitting or discomfort or tension in your pelvis and getting an evaluation by a pelvic floor therapist may help to head off any potential issues before they become chronic.
Outlook for recovery/recurrence
While it is still a complicated, multifaceted condition that requires some work to properly diagnose, the prognosis for people with prostatitis is relatively good. Antibiotics are very effective in curing acute prostatitis. Antibiotics can relieve symptoms in 30 percent to 60 percent of men with chronic bacterial prostatitis.
Research shows that up to 80 percent of men report relief after being treated for their particular symptoms using the UPOINT system.
FAQs
What are the four most common signs or symptoms of prostatitis?
The main signs or symptoms of prostatitis include:
- Erectile dysfunction
- Pain in the penis, testicles and perineum that may refer to the lower back or hips
- Painful ejaculation
- Urinary tract difficulties, including painful urination, frequent urge to urinate, and a weak stream or a stream that starts and stops
What does prostatitis feel like?
Prostatitis comes with a wide variety of symptoms, so it may feel different to anyone who has it.
Some common symptoms include having a constant, low ache in the area inside your pelvis behind your penis and testicles; pain when urinating; pain when sitting for a long time; constant tension in the perineum, lower groin or lower back; and pain when engaged in sexual activities and ejaculating.
Is prostatitis a serious condition?
It depends on the type of prostatitis. And it's important to note at this point that prostate cancer and prostatitis are two very separate conditions.
A round of antibiotics usually clears up acute prostatitis. On the other hand, chronic prostatitis can lead to serious complications, such as bacterial blood infections, abscesses on the prostate and more.
Chronic pelvic pain syndrome (CPPS) can have a serious impact on a person's quality of life if left untreated.












