Epididymitis: Myths & Misconceptions
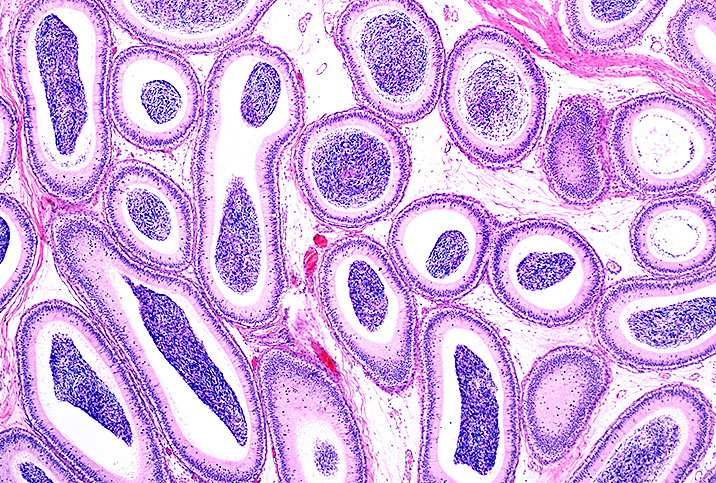
The epididymis is a 20-foot-long coiled tube, located at the upper back of each testicle inside the scrotum, that is responsible for carrying sperm from the testicles. It takes about two weeks for sperm to make that journey, during which time they mature until they're ready to be mixed with seminal fluid and expelled when a man ejaculates.
When the epididymis gets inflamed, it causes a condition called epididymitis, resulting in redness, tenderness and swelling of the epididymis as well as the overlying scrotal tissue. There also may be an increased amount of fluid within the scrotum due to inflammation.
Epididymitis can be a serious condition, especially when it lasts longer than six weeks. The pain and swelling of the epididymis can spread to the testicles, which can also become inflamed, resulting in a condition called epididymo-orchitis.
But as common as epididymitis is—more than half a million men in America are diagnosed with the condition each year—there are many misconceptions about epididymitis and its effects.
Myth: Epididymitis is always caused by sexually transmitted infections (STIs).
Reality: While STIs can be the underlying cause of epididymitis, there are others. It's well known that sexually transmitted diseases (STDs), especially chlamydia and gonorrhea, can prompt a bout of epididymitis. Older people may think this association with STDs makes epididymitis a disease for only younger people to worry about, but it can affect a range of age groups from children to seniors. Older patients may get epididymitis from an infection of the bladder, kidneys, urethra or prostate (prostatitis).
Here are some other potential causes of epididymitis:
- Blockage in the urethra
- Bladder or urinary tract infection (UTI)
- Enlarged prostate
- Traumatic groin injury
- Mumps
- Tuberculosis
- E. coli bacteria
Myth: The only symptom of epididymitis is swollen, tender testicles.
Reality: Epididymitis can present with a wide array of symptoms. It's true that the slow onset of pain, swelling and tenderness in the testicles is usually the first symptom of epididymitis that men notice. However, if it's left untreated and symptoms are allowed to get worse, epididymitis can result in:
- Chills
- Low-grade fever
- Enlarged lymph nodes, especially in the groin
- Painful ejaculation and pain during sex
- Unusual penile discharge
- Frequent urination
- Blood in semen
Some patients can have a chronic version of epididymitis in which they may feel less pronounced symptoms or less obvious overlying swelling of the scrotum, and the pain and symptoms may feel more internal.
Myth: Epididymitis affects only sexually active men.
Reality: Even non-sexually active children, teenagers and older men can contract epididymitis.
While the most common age cohort for contracting epididymitis is men and boys 14 to 35 years old, there is such a thing as pediatric epididymitis: In those cases, boys with the condition have usually experienced groin trauma or a urinary tract infection that led to epididymitis.
In older men who are no longer sexually active, epididymitis can also stem from urinary tract infections, as well as:
- An enlarged prostate
- Using a catheter for urination
- Recent surgery on the urinary tract
- Using a heart medication called amiodarone
Males of any age should always talk to their doctor or get a referral to a urologist whenever they experience abnormal pain or unresolved symptoms involving the urinary/reproductive tract.
Myth: Epididymitis is easily diagnosed.
Reality: Other conditions related to the testicles can complicate the diagnosis of epididymitis.
Testicular torsion is a particular concern, especially when younger men and teens present with swelling and pain in the testicles.
While epididymitis is a condition that isn't tremendously serious, at least in the short run, testicular torsion is a four-alarm fire that may need emergency surgery or risk the strangulation of a testicle. A urologist may order an ultrasound to check for blood flow to the testicles to differentiate a case of epididymitis from testicular torsion.
An ultrasound gives an anatomic evaluation of the testes, epididymis and scrotal sac. It's a quick, low-risk test to provide emergency findings such as torsion, a twisting of the testes about the cord containing the blood vessels supplying the testicle. Loss of blood flow can lead to all or part of the testicle having tissue death, which requires surgical untwisting and assessment for the viability of the testes.
Myth: Epididymitis can go away on its own.
Reality: While symptoms of untreated epididymitis may fade, it is very unlikely to go away entirely without treatment.
Epididymitis is an infection that requires antibiotics to be fully treated, especially when there are possible long-term complications from letting it go untreated:
- Chronic epididymitis
- Testicle shrinkage
- Development of a fistula, or abnormal opening, in the scrotum
- Infertility
- Possible spread to other parts of the reproductive/urinary tract
While epididymitis is relatively common and benign when definitively diagnosed and treated early, it can lead to more serious complications if left untreated, so seeing a medical clinician is important to accurately diagnose the condition and rule out other possible underlying issues. It's safe to say that any testicular pain is worthy of a doctor visit just to be on the safe side, especially with young men and teens.