Urinary Incontinence in Menopausal Women Is Common

During the menopausal transition and postmenopause, many women struggle with hot flashes, vaginal dryness, slowed metabolism and other side effects that you've probably heard about. But you might not consider urinary incontinence (UI), which can seriously affect a woman's day-to-day life.
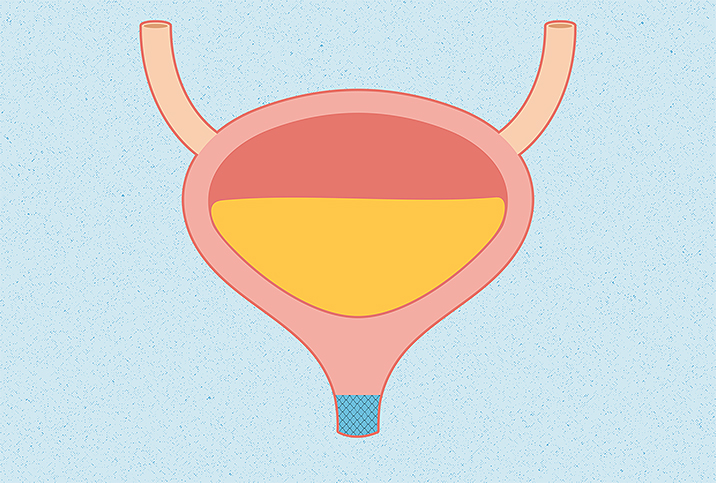
Urinary incontinence occurs when someone can't control their bladder and leaks involuntarily. This can happen during intercourse, after sneezing and coughing or even when lifting something heavy. Urinary incontinence affects more than 50 percent of menopausal women. And while this condition is more prevalent in all people as they age, UI affects women twice as often as men.
What causes urinary incontinence during the menopausal transition?
In general, urinary incontinence is caused by the weakening of the muscles that help the bladder hold or pass urine. As with pregnancy and childbirth, women during perimenopause and postmenopause will experience a weakened bladder.
"Menopause specifically is more associated with decreased estrogen to the genital tissues, including the urethra and bladder, which can lead to more frequent urination, pain with urination and urinary tract infections," said Kelly Culwell, M.D., an OB-GYN and nationally renowned women's health expert who goes by Dr. Lady Doctor.
Decreasing estrogen affects pH levels in the vagina, which control infection-causing bacteria. The vagina is naturally slightly acidic, and with a change in pH level, women may experience more urinary tract infections.
Hormonal changes, such as those that occur during menopause, may also trigger lichen sclerosis, which can cause urinary incontinence. "This is a dermatologic skin condition where the skin becomes thin, fragile and pale, often accompanied by itching or burning sensations of the vulva, perineum and perianal areas," said Staci Tanouye, M.D., an OB-GYN, Poise partner, and physician in Jacksonville, Florida.
How will a doctor diagnose urinary incontinence?
Your doctor will ask you when and how often you experience incontinence, and ask for a thorough past medical and obstetric history. According to Seattle-based Sarah de la Torre, M.D., an OB-GYN with Joylux, some questions may include the following:
- Do you "leak" urine while lifting, sneezing, laughing, coughing or having sex?
- Do you feel like your bladder is never completely empty?
- Do you have a hard time making it to the bathroom in time?
Your doctor may also ask you to keep a daily bladder diary to get a clearer idea about your condition. Then they will do a specialized exam that can determine what type of incontinence you have, which will determine treatment. Some exams may include:
- Urine samples to check for bacteria.
- Urodynamics to test the function of the bladder muscles.
- Cystoscopy to look inside the bladder, or an ultrasound/CT scan to look for cancers and other structural causes.
How will a doctor treat urinary incontinence?
If a doctor confirms that you are experiencing an overactive bladder, they may recommend the following treatments, according to Tanouye:
- Pelvic health physical therapy: Work with a pelvic health physical therapist as a noninvasive option. They can provide exercises to restore strength in the pelvic area.
- Bladder training: Follow a urination schedule to help get the bladder used to less frequent trips.
- Medication: Relax the bladder muscles and nerves through medicine. Before taking medication, it's important to note that you should always consult with your primary healthcare provider.
- Products for comfort: While experiencing and/or treating excessive urination, it can be helpful to stay prepared for leaks or urgencies. Keep pads, panty liners and fresh underwear on hand.
Is preventing or reversing the issue possible?
"Avoiding risk factors for incontinence—such as obesity, smoking and, if you have diabetes, keeping your blood sugar under control—is important," Culwell said.
It's worth noting that pregnancy alone can cause urinary incontinence and increase future risk, "but it is even more increased if injuries to the pelvic floor happen during vaginal birth," she added.
Thankfully, there are exercises you can do to help. "Pelvic floor strengthening exercises (e.g., Kegels) can also help keep the pelvic floor strong to prevent incontinence, but they need to be done correctly," Culwell said. A pelvic floor physical therapist and some OB-GYNs can help teach you the correct way to do these exercises.