Your Chronic Yeast Infections Could Be Lichen Sclerosus
Genital itching and discharge. It's a topic no one wants to think about—let alone deal with—but it's also a symptom that can have a debilitating impact on your quality of life.
For women especially, many cases of genital itching—especially when accompanied by other symptoms, such as vaginal discharge—are attributed to yeast infections. But if you're having chronic, severe itching that doesn't resolve with yeast infection treatments, you may be dealing with a different condition altogether: lichen sclerosus.
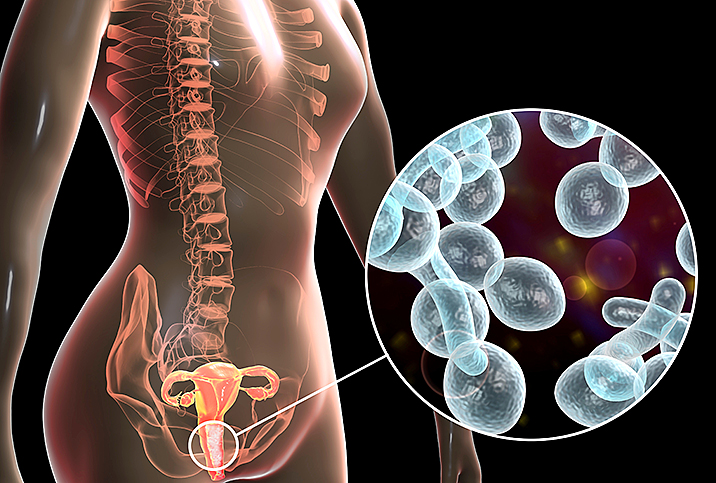
Lichen sclerosus is an autoimmune skin disorder, vs. a yeast infection, which is caused by a pathogen. So unfortunately, antifungals won't help.
What is lichen sclerosus?
As Cedars-Sinai hospital explained, lichen sclerosus is a chronic skin condition that primarily affects the skin of the vulva and labia, as well as around the anal area.
It can occur in men, women and children, but is most common in women who have gone through menopause. However, Crystal Murphy, M.S., CNM, APRN, noted she has seen the condition even in young girls.
Unfortunately, when it comes to issues like genital itching, it can be difficult for people to seek out professional help.
"You'd be surprised how long people actually will put up with something because they don't want to go to the doctor—we're all guilty of it," said Murphy, who works as a midwife at Tru Birth Center in Lakewood, New Jersey.
The primary symptoms of lichen sclerosus are:
- Pale, almost white color to the skin
- Skin appearing more thin
- Severe vulvar and anal itching
- Skin blisters and tears
- Pain with sex
- Trouble urinating
It's not entirely clear what causes lichen sclerosus, but Murphy explained it's thought to be from factors that include genetics, hormonal changes, previous infections or a combination of many different things.
In most cases, she said, the patient seeks help for itchiness and discharge, is treated for a yeast infection, but then when that doesn't help and the problem persists—or even worsens—they move on to investigating other causes. A skin biopsy is the only way to confirm the diagnosis of lichen sclerosus.
Lichen sclerosus vs. a yeast infection
It can be difficult to distinguish between the two problems at first, because both have similar symptoms. For instance, both lichen sclerosus and yeast infections will lead to an inflammatory response in the body, which causes severe itching in the vulvar areas. Additionally, both may be accompanied by vaginal discharge.
However, while the discharge associated with a yeast infection is a sign of an internal issue (the yeast infection itself), with lichen sclerosus, the discharge is a byproduct of damage caused by scratching. Murphy explained that anytime you have itching, the natural response is to scratch the itch, but because most women have fingernails, the scratching can cause small nicks and tears in the skin.
These tiny abrasions can get infected and worsen the inflammatory response. As a result, the body increases its discharge in an attempt to heal the body and fight off infection. And then, of course, the increased discharge may also exacerbate irritation and cause even more itchiness, so a vicious circle is created.
Because lichen sclerosus is a skin condition, it can even eventually narrow the vaginal and urethra openings and distort the appearance of the labia as well.
In addition to the fact that a yeast infection treatment won't be effective, one of the key signs you could be dealing with lichen sclerosus is that the appearance of the skin changes with whitish "plaques," or patches, on the skin. The name "lichen" even alludes to this, as it refers to white, crusty lichens that grow on rocks.
"The tissue looks a little bit different—it gets really pale," Murphy described. "The other sign is, depending on how long they've had it, is that the labia majora kind of starts to disappear if they've had it long enough."
Because lichen sclerosus is a skin condition, it can even eventually narrow the vaginal and urethra openings and distort the appearance of the labia as well. "It can actually be physically deforming for the woman because she will no longer look the same as what she used to look like," Murphy added.
Treatment for lichen sclerosus
Unfortunately, there is no cure for lichen sclerosus and it is a chronic condition. So, treating lichen sclerosus is focused on managing symptoms such as itching and discharge.
Treatment usually includes beginning with a steroid cream to apply on the skin, Murphy said. Then, if the cream doesn't work, a trip to a dermatologist may be warranted. She also added some other treatment options may include:
- Ultraviolet light therapy
- Retinoids
- Steroid injections
- Antidepressants for vulvar pain
- Ointments
In very rare cases, surgery may also be an option, but Murphy noted surgery doesn't tend to be effective, because even if the patches are removed, they usually come back. Additionally, surgery may lead to vaginal scarring, which can cause its own complications on top of the lichen sclerosus.
Seeking help for lichen sclerosus
As we mentioned earlier, seeking help for conditions that involve the genitals—especially with something "embarrassing" like extreme itchiness—can be challenging. And even more challenging is the fact that even if you finally do work up the nerve to go to the doctor, not all practitioners are trained on diagnosing and treating lichen sclerosus.
However, the important thing to remember is if you are dealing with discomfort that is affecting your quality of life, you deserve to find someone who can help you. "You should not be living in constant irritation," Murphy said. "Sometimes people feel like they want to take a hairbrush to that area—that is not normal."
Murphy stressed if you've seen your primary care provider and have been treated with creams and your symptoms still aren't getting better, you should follow up and book an appointment with someone else. Not all primary care doctors are specialists, so the condition may not be apparent to all practitioners. If necessary, you could even book an appointment with the Centers for Vulvovaginal Disorders—which has offices in Washington, D.C., and New York City—for specialized treatment.
"If you're not getting answers, then it's time to go see somebody else," Murphy said. "Don't ever be afraid to get a second opinion."