When does Urinary Incontinence Require Surgery?
Urinary incontinence is a significant health issue in America and can have a considerable impact on your social life. In women, the prevalence of moderate to severe urinary incontinence ranges from 3 percent to 17 percent, whereas men have a much lower prevalence at 2 percent to 11 percent. In all cases, the rate increases rapidly at age 70 and above.
Safe and successful
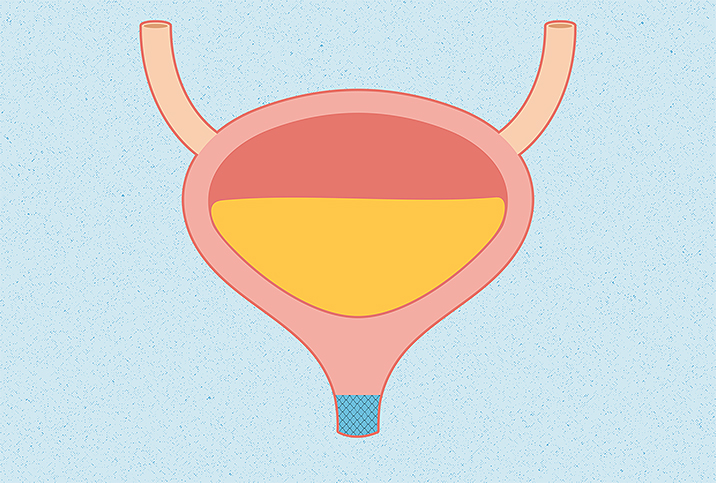
Various treatments are available, but one of the safest and most successful options is the bladder sling. Surgically placed by a urogynecologist or urologist using laparoscopy—an operation performed in the abdomen using small incisions with the aid of a camera—a bladder sling offers support for the urethra. By lifting the bladder neck, or the junction of your bladder and urethra, the pressure applied by the sling's support aids in urine retention and controlled release.
The bladder sling itself may be naturally or synthetically derived. A synthetic sling is composed of a body-safe plastic mesh that deteriorates over a period of up to five years. A natural sling is created with ligaments, muscles or tendon tissue taken from the patient or farmed from an animal (typically a pig) and can last indefinitely.
Ideally, if the bladder sling is constructed from another part of the patient's body, this lowers the chance of the body rejecting the foreign device, which could result in infection. Infection often requires longer and more complex surgery that calls for constructing a new sling and the removal of the infected implanted sling, which may have caused other regional damage or scarring from inflammation.
When you need a bladder sling
Despite an involved recovery necessitating a catheter, bladder slings have been found to be very effective in combating stress-induced urinary incontinence.
The stress referred to here is the physical stress placed on the bladder. For example, when a person sneezes, laughs intensely or even goes running, urine can leak from the urethral sphincter. The urethral sphincter, like the more commonly known anal sphincter, is a group of different types of muscles organized as an internal sphincter and external sphincter. Together, they regulate the flow of urine from the bladder to the urethra, and, in men, are also involved in ejaculation.
However, emotional stress can also cause uncontrollable urine flow, even in young, healthy adults. If a problem in your emotional life consistently goes unaddressed, the body may find other outlets to express itself.
While slings might be occasionally necessary for younger patients experiencing incontinence, a bladder sling is most commonly prescribed after a prostatectomy—the removal of the prostate, typically because of cancer—or a hysterectomy.
A bladder sling may also be a necessary measure after vaginal prolapse. The rate of vaginal prolapse becomes more prevalent after a hysterectomy, regardless of why you had the procedure in the first place. A bladder sling may also be prescribed following pelvic or genital cancer to help the patient recuperate and return to normal bladder function.
Bladder sling surgery can interfere with childbearing, so health professionals usually recommend a number of noninvasive techniques for premenopausal people suffering from urinary incontinence.
The alternatives
Bladder sling surgery isn't the only solution to urinary incontinence, and it's not even the only invasive procedure.
Overactive bladders can be treated with electrical stimulation, in a similar way to a heart benefiting from a pacemaker. A stimulator attached to an electrode-tipped wire can be attached to the sacral nerve, or the network of nerve fibers extruding from spinal nerves that control the pelvis and lower body.
For a less invasive method, a physician may recommend pelvic therapy, which isn't confined to Kegel exercises. Certain yoga poses and lower body exercises can help (yet another benefit of doing squats), and physical therapists (PTs) can help women work with dilators, or sets of tube-shaped devices that gradually stretch clenched vaginas and strengthen weakened pelvic floors. The work is emotional as well as physical.
Certified nurse-midwife (and this author's mother) Adrienne Crowe said anyone suffering incontinence should start with small solutions first.
"Surgery should never be the first solution to a health concern, even one as uncomfortable as urinary incontinence," Crowe said. "It's a fact that pelvic floor health in either sex is directly linked to incontinence, but it's a muscle that can be worked. First and foremost, an individual should evaluate their caffeine intake and practice Kegels by interrupting the flow of urine temporarily—those are the muscles you want to flex, not your upper thighs or glutes."
While it's dangerous to wave off health concerns as a result of less-than-ideal circumstances, evaluate whether you've pursued these more conservative measures before considering surgery. Be sure to discuss the decision with your OB-GYN, physician, urologist and other people on your team of care. More opinions will help you make the best choice.
Urinary incontinence may stem from a slew of causes, but only certain cases are treated with bladder slings. If you're experiencing loss of bladder or rectal control, it's recommended you discuss those issues with a physician. And keep in mind the origins may be strictly physical or may be psychosomatic and lead to talk therapy rather than surgery.
Always be patient with yourself and try to be as kind as you can. While nothing feels as isolating as incontinence, many more people than you might think have been exactly where you are. Reach out to your family and friends and to support groups, online and in person.