Epididymitis Is Likely Going to Require Antibiotics

Many conditions seen by urologists can be complicated and/or unique. They often correlate or coincide with various forms of infection that may require antibiotic treatment to resolve the issue or, at the very least, ease the patient's suffering.
One such condition is called epididymitis, a potentially painful and problematic medical experience which can be differentiated into multiple categories.
The basics of antibiotics and epididymitis
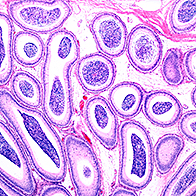
The epididymis is a coiled tube at the back of each testicle that stores and carries sperm. Whenever the epididymis becomes inflamed or swollen, it can cause intense pain in the testicle.
"There are kind of two groups of epididymitis," said Stan Honig, M.D., a urologist and the director of men's health at Yale School of Medicine in New Haven, Connecticut. "One is what's called infectious epididymitis, which is a much more acute course, meaning that it's [linked to] severe pain, it's associated with some urinary symptoms sometimes, and the testicle and the epididymis can swell up significantly. And those are the ones that respond well to antibiotics and usually get better without a problem."
It's less common for antibiotics to be employed in the treatment of the second type of epididymitis, though in some cases, Honig said parallel or underlying infections may necessitate antibiotics, as well.
"The second group is…almost like a chemical or an inflammatory epididymitis where they just have a discomfort; they may have kind of a 'blue ball syndrome' where their epididymis gets congested," he said. "And most of the time that type of thing is self-limited. It can get better with releasing an ejaculate or it can get better with just anti-inflammatory medicine. Sometimes there can be an underlying, mild infection, so we sometimes will start those people on the antibiotics, as well."
Regardless of the epididymitis type or whether the symptoms end up being epididymitis at all, Honig emphasized the importance of medical support when dealing with infectious or noninfectious conditions in that area of the body, just to make sure it's nothing serious.
How doctors check for epididymitis
Epididymitis can be linked to a number of different infection types, so the antibiotics used to treat the condition, if necessary, can vary.
"It may often be associated with a urinary tract infection, a standard urinary tract infection; in other words, a bladder-type infection," said Robert Moldwin, M.D., the director of the Pelvic Pain Treatment Center at the Arthur Smith Institute for Urology in Lake Success, New York. "It may also be associated with a chronic infection within the prostate gland, because the tubes from the epididymis obviously have to eventually connect up with the prostate, so any infection that might be smoldering in the prostate gland, theoretically, can backflow to the epididymis and testicle."
The possibility of things flowing in the wrong direction and transporting unwanted infectious or otherwise harmful materials has special relevance to complications associated with sexually transmitted diseases (STDs) and infections (STIs). The germs and microorganisms are moved backward and can cause an infection at their final stop. Moldwin described the movement from the urethra all the way up through the prostate, through the vas deferens and finally to the epididymis.
"Those are our first concerns," he said. "And if there's a [medical] history and physical examination, and certainly laboratory examinations that are confirmatory, we go ahead and there's no question that antibiotic therapy would clearly be indicated."
Infections can be difficult to identify even when consistently placed pain persists for the patient. Moldwin mentioned that different specialists are typically trained to think in different lanes in terms of medical tools, knowledge, screening methods and resources, and sometimes the treatment of pain and/or discomfort takes priority while the definitive sources of irritation remain elusive. In the end, is it even an infection?
The tricky thing is it's not wise to avoid or neglect the use of antibiotics. But the more information you can have at your disposal as a patient working in collaboration with your doctors, the better.
Getting to an epididymitis diagnosis
The bottom line is a doctor's opinion and guidance are vital to treating something like epididymitis with antibiotics and other measures, especially when you consider the multitudes of possible combinations pertaining to both the problems at hand as well as their solutions.
Doctors can't do very much with what they don't find, except, hopefully, narrow in on the actual source of the pain or condition they are treating. By the time a patient ends up in the care of someone like Moldwin for any number of conditions, they may have already attempted several treatments and avenues of investigation with lackluster results available beyond the speculative.
"Epididymitis is the same way," Moldwin said. "Like I say, the types of patients I see are not the patients who've actually done well on antibiotics, they're the patients who've been refractory. They still have epididymal or testicular pain, and we're trying to figure out what the source is. But the bullet points here for the standard patient who comes in with epididymitis is that yes, antibiotics are often one of the first lines of management, even as empiric therapy for these conditions."