Additional Chemo May Cut Risk of Cervical Cancer Death by One-Third

Key Points
- In its early stages, cervical cancer typically doesn't cause any symptoms, so diagnosis relies on screenings such as Pap tests, which many women forego. As a result, when many are eventually tested, they are diagnosed with locally advanced or advanced cervical cancer.
- The standard-of-care treatment for locally advanced cervical cancer has been chemotherapy plus radiation.
- A 2023 study suggests giving patients a short course of induction chemotherapy before each chemoradiation session could cut the risk of death or cancer recurrence by about one-third.
Discussions about cervical cancer typically focus on prevention and screening. It makes sense since the disease has a high five-year relative survival rate when detected in its early stages. However, as with all cancers, the risk of death climbs once the tumor has grown or spread.
A 2023 study offers hope for people with locally advanced disease. Its findings suggest adding already-approved drugs to the standard treatment regimen could cut the risk of death or cancer recurrence by about one-third.
What did the study find?
The findings were presented at the European Society for Medical Oncology congress in October 2023. In the study, known as INTERLACE III, researchers followed 500 cervical cancer patients from hospitals in the United Kingdom, Mexico, India, Italy and Brazil for 10 years.
Most participants had a "locally advanced" form of the disease, meaning the tumor was larger than 4 cm but was still confined to the cervix or had spread to surrounding tissues but hadn't infiltrated other parts of the body, according to Cancer Research UK.
Half of the patients received chemoradiation (CRT)—a combination of chemotherapy and radiation—the standard-of-care treatment for cervical cancer. The other patients received a short course of induction chemotherapy (IC) before each CRT session.
The researchers found that most participants who received IC and CRT survived longer than those treated with CRT alone. After five years, 80 percent of those who received both treatments were alive, compared to 72 percent of those who only received CRT.
The combined treatment also reduced the risk of recurrent cervical cancer. Seventy-three percent of patients who received CRT and IC hadn't seen their cancer return or spread, compared to 64 percent of those who had received CRT alone.
"Our trial shows that this short course of additional chemotherapy delivered immediately before the standard CRT can reduce the risk of cancer returning or death by 35 percent," said Mary McCormack, M.B.B.S., M.Sc., a consultant clinical oncologist at University College London Hospitals and the trial's lead investigator, in a recent press release. "This is the biggest improvement in outcome in this disease in over 20 years."
The drugs used in IC—carboplatin and paclitaxel—are inexpensive, accessible and already approved for use, so they could easily become part of standard cervical cancer treatment for patients everywhere, study authors said.
"These findings are very exciting for the treatment of women with a disease which is severely lacking in options," said Manolis Tsatsas, M.D., the director of gynecologic oncology at Northwell Staten Island Hospital in New York, who was not involved in the study. "We are anxiously awaiting to hear the full results of the trial in the hope it could be adopted in the United States in the near future."
The findings are a significant advance in treatment, according to Roberto Vargas, M.D., a gynecology oncology specialist at Cleveland Clinic and the developmental therapeutics program at Member Case Comprehensive Cancer Center.
"The trial addresses a cervical cancer population that is not a candidate for surgery and is traditionally treated with radiation and chemotherapy administered at the same time," said Vargas, who was not involved in the study. "This treatment approach has remained the same over the past three decades.
"While we have been successful at reducing the incidence of cervical cancer, we have not significantly impacted the survival rates of the cancer once it is diagnosed."
Recommended
- Can You Get Cervical Cancer if You Don't Have Sex?: Most cervical cancer cases are caused by HPV, but a small risk exists for people who aren't sexually active.
- More Cases of Cervical Cancer Linked to HPV Than Previously Thought: A new study reaffirms a strong link between this gynecological cancer and human papillomavirus.
- Raising Awareness: TogetHER on Eliminating Cervical Cancer Worldwide: Giddy talks to executive director Heather White about funding global access to resources.
Why has CRT been the standard treatment until now?
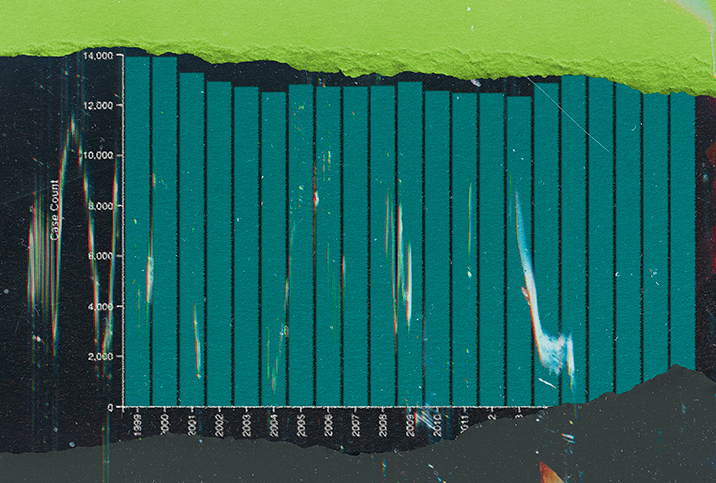
Radiation alone was the predominant treatment for cervical cancer for nearly 100 years until 1999 when concomitant chemotherapy became the standard of care, Tsatsas explained.
"Since then, a weekly dose of chemotherapy along with radiation treatment has shown the best outcomes for patients with locally advanced disease," Vargas said.
Before the INTERLACE III study, prospective trial data was lacking to indicate that the addition of carboplatin and paclitaxel would impact survival rates or cut the risk of cervical cancer return.
Another recent study, the OUTBACK trial published in May 2023 in The Lancet, looked at multiagent regimens given after chemoradiation. Findings suggest that the approach did not improve outcomes, according to Vargas.
"This highlights that it's not just the fact they are receiving more treatment that leads to better outcomes but that the order of therapy matters," he added. "We are learning more each day about how the evolution of cancers through treatment may impact when and how we can utilize existing drugs to achieve the best outcomes."
"The purpose of IC is to shrink solid tumors to improve the effectiveness of radiation or surgery and decrease the risk of cancer cells spreading to other body parts," said Joshua Cohen, M.D., a gynecologic oncologist and medical director of the gynecologic cancer program at City of Hope Orange County in California.
Other evidence suggests that treating cancer with immunotherapy could improve outcomes for people with cervical cancer. More research is needed to determine what patients will benefit most from different treatments.
"With additional chemotherapy, there is an added risk of toxicity for patients, including neuropathy, bone marrow suppression, fatigue and constipation," Cohen said. "Many of these side effects are transient, but there can be long-lasting side effects sometimes. When we recommend treatments to patients, we want to ensure that the benefits are worth the risk."
Protecting Your Fertility During Ovarian Cancer Treatment: Knowing yourreproductive options can preserve the possibility of starting or growing a family.
What are the chances of being diagnosed with cervical cancer?
Every year in the United States, about 11,500 new cases of cervical cancer are diagnosed, and roughly 4,000 patients die, according to the Centers for Disease Control and Prevention (CDC).
Usually, cervical cancer is diagnosed in women between the ages of 35 and 44, though more than 20 percent of cases are diagnosed after age 65, per the American Society of Clinical Oncology (ASCO).
"The human papillomavirus [HPV] accounts for about 95 percent of cervical cancers," Tsatsas said.
HPV affects nearly all sexually active people, regardless of sex, gender or sexual orientation, according to the National Cancer Institute (NCI). Of the many types of HPV, 12 can lead to cancer.
Most people with HPV will not get cancer, but roughly half of infections are one of those high-risk subtypes, per the NCI and CDC.
The immune system clears most HPV infections within a year or two without any long-term ramifications. Those that persist for several years, however, can lead to cellular changes that can eventually cause cervical cancer or other cancers, including anal, oropharyngeal, penile, vaginal and vulvar.
"It will generally take many years for this virus to cause dysplasia (pre-cancerous changes) and then reach the cancer stage," Vargas said.
Women who get an HPV infection in their early 20s may not develop cervical cancer until their mid-30s or later, according to Tsatsas.
"Age isn't the only risk factor," Cohen said. "Folks who are immunocompromised and those who smoke or have obesity are also more vulnerable."
When cervical cancer is diagnosed in its early stages, the five-year relative survival rate is 92 percent, according to ASCO.
The five-year relative survival rate drops to 59 percent for people who receive their cervical cancer diagnosis after the disease has spread to nearby tissues, organs or regional lymph nodes. For people who are diagnosed with advanced cervical cancer that has metastasized—or spread to distant parts of the body—the five-year relative survival rate plummets to 17 percent.
Only 44 percent of people are diagnosed with early-stage cervical cancer, per ASCO. Recent research indicates that rates of terminal cervical cancer are rising for older women, who tend to be diagnosed with advanced disease.
Student Is Diagnosed With Cancer After Years of 'Medical Gaslighting': The patient says one doctor disregarded her painful abdominal symptoms as thong irritation.
How can you prevent cervical cancer?
Vargas noted that cervical cancer is preventable, and the HPV vaccine is the most effective way to avoid it.
"Clinical data show that vaccination before the age of 17 reduces the risk of cervical cancer by 88 percent, with patients vaccinated between the ages of 17 and 30 seeing a 53 percent reduction in risk," Vargas said.
"Condom use can also reduce the likelihood of HPV transmission by about 70 percent," Tsatsas said.
Other measures that can help to reduce cervical cancer risk include getting regular Pap smears and HPV screenings.
There's no cure for HPV, but these tests can significantly cut the risk of abnormal (pre-cancerous) cells turning into cancerous ones. If an HPV screen detects a high-risk strain, a doctor can follow up with monitoring and further testing. If a Pap smear indicates pre-cancerous cells, procedures like the loop electrosurgical excision procedure (LEEP), laser ablation or cryotherapy (freezing) can remove them.
"In the U.S., most patients with cervical cancer have either never been screened or haven't had a screening in five years at the time of diagnosis," Tsatsas said.
Besides the notion that only promiscuous women and men get HPV or that men cannot get the virus, one of the more dangerous cervical cancer myths is that all people who get HPV will experience symptoms.
Generally, HPV doesn't cause any symptoms, though low-risk types unaffiliated with cancer can lead to genital warts, according to the NCI. Likewise, cervical cancer is frequently asymptomatic in its early stages, which is why testing is crucial.
"As a gynecologic oncologist who sees many patients with cervical cancer, I strongly encourage including HPV vaccination in your routine vaccination schedule and getting cervical cancer screenings as your physician recommends," Cohen said.
The bottom line
Methods of treating cancer continue to evolve as new science and technology emerge. Even so, prevention remains by far the best way to reduce the risk of cervical cancer.
Talk to your healthcare provider for more information about your risk and screening recommendations.