A Guide to Vulvar Cancer: Risks, Symptoms and Treatments
The American Cancer Society estimates that 6,120 women will be diagnosed with cancers of the vulva in 2021, and about 1,550 will die because of the disease.
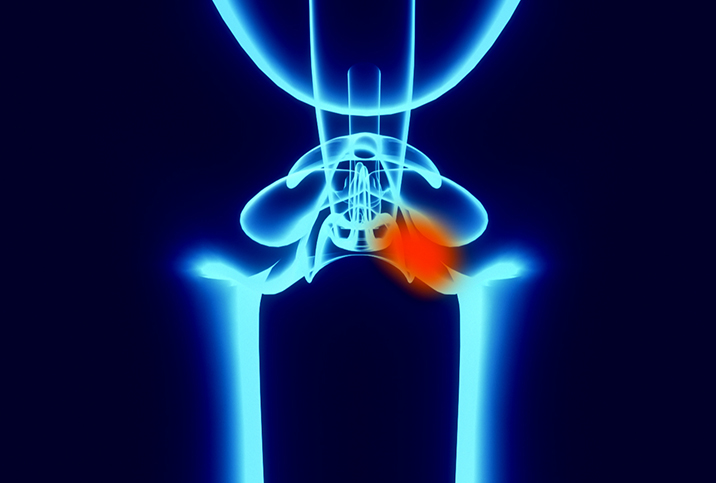
Vulvar cancer is a relatively uncommon disease that usually forms as an itchy lump or sore on the vulva, which is the outer surface of skin around the urethra and vagina, including the clitoris and labia. It’s important to be aware of the signs of vulvar cancer, so you can consult a doctor if you experience any symptoms of the disease, which include:
- Persistent itching
- Pain on or around the vulva
- Unexplained bleeding
- Changes in the color or texture of skin on the vulva
- The appearance of lumps, wart-like bumps or open sores
Risk factors of vulvar cancer
In general, cancer occurs when the DNA in cells begins to mutate, causing the cells to grow and divide rapidly. When this happens, healthy cells start to die and the cancerous cells proliferate, often leading to the formation of tumors.
While the exact causes of cancer, vulvar cancer in particular, remain unclear, data have shown that some factors may increase an individual’s chance of developing the disease. One risk factor of vulvar cancer is growing older. Though the disease can occur at any age, it is most prevalent among older women, with 65 being the average age at diagnosis, according to the Mayo Clinic.
Women who have been exposed to human papillomavirus, a sexually transmitted infection commonly known as HPV, are also more at risk of vulvar cancer. Although in most cases there are no symptoms of HPV and it can go undetected for years, a vaccine is now available to protect against it.
As is the case with other cancers, smokers are more at risk of developing vulvar cancer, as are people who have a weak immune system. A rare precancerous condition called intraepithelial neoplasia, involving the presence of abnormal cells in the vulva, most likely never progresses but can develop into invasive vulvar cancer. The precancerous condition can also be tied to an HPV infection.
Another uncommon condition called lichen sclerosus, which causes the skin of the vulva to become thin and itchy, is a vulvar cancer risk factor.
How to treat vulvar cancer
A doctor may recommend one or more treatments for vulvar cancer, depending on its type, location and stage.
Vulvar cancer presents as two types: vulvar squamous cell carcinoma and vulvar melanoma. Vulvar squamous cell carcinoma originates in the thin, flat cells that line the surface of the vulva and accounts for most cases of vulvar cancer. Meanwhile, vulvar melanoma starts in the pigment-producing cells in the skin of the vulva.
Treatments for vulvar cancer vary and include the following:
- Surgery. Depending on the case, a doctor might recommend a vulvectomy, which includes the partial or full removal of the vulva and is typically offered for larger cancers. Surgical options also include lymph node removal as well as excision, which entails the removal of cancerous tissue and a smaller amount of surrounding healthy tissue.
- Radiation. High-powered energy beams such as X-rays and protons are used to kill cancer cells.
- Chemotherapy. A drug treatment, chemotherapy is often used in combination with radiation to shrink or kill cancer cells.
- Immunotherapy. A patient’s own immune system is activated to help fight against cancer cells.
The earlier vulvar cancer is detected, the better the chance it can be successfully treated. According to the American Cancer Society, people who start treatment for vulvar cancer before it has spread have a five-year survival rate of 86 percent.
How to prevent vulvar cancer
Women can’t prevent vulvar cancer altogether, but they can take steps to lessen their risk of getting the disease.
One of the best ways to reduce the risk of vulvar cancer is to protect yourself against HPV by getting the HPV vaccine. Medical professionals recommend males and females get the HPV vaccination at 11 or 12 years old, and up until 26. (Adults ages 26 through 45 may consider the vaccination if they weren’t vaccinated adequately before, but they should consult their healthcare provider before making this decision.)
If you’ve received the vaccine, you can further reduce your risk of getting HPV by using a condom every time you have sex, though this alone cannot fully protect you from HPV, because it is transmitted by intimate skin-to-skin contact.
Getting regular pelvic exams as part of yearly preventive health checkups can ensure you and your primary doctor can monitor your reproductive organs and catch and treat anything out of the ordinary as soon as possible.

















