Late-Stage Cervical Cancer Rates Are on the Rise
Rates of advanced-stage cervical cancer are on the rise in the United States, according to a new study published in the International Journal of Gynecological Cancer.
In 2022, an estimated 14,100 people will be diagnosed with invasive cervical cancer and about 4,280 will die from the disease, according to the American Cancer Society (ACS). It's the fourth most common cancer among women worldwide and the sixth most prevalent among women in high-income countries.
With early diagnosis and intervention, cervical cancer is highly treatable, with a five-year survival rate of 92 percent, according to the American Society of Clinical Oncology (ASCO). But when the disease does progress, it's deadly. The five-year survival rate drops to 18 percent when advanced-stage cervical cancer spreads to other parts of the body.
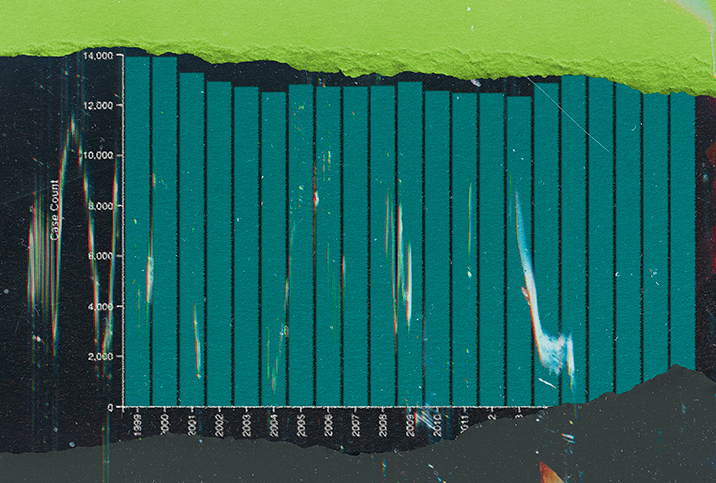
In the study, researchers obtained data for 2001 to 2018 from the U.S. Cancer Statistics program to assess the cervical cancer diagnoses of 29,715 women spanning multiple demographics. They used data from the Behavioral Risk Factor Surveillance System and TeenVaxView to evaluate screening and vaccination practices. Overall, they found a 1.3 percent year-over-year increase in metastatic (late-stage) cervical cancer.
Experts say this finding indicates a distinct need to prioritize HPV vaccinations, cervical cancer screening and increased access to quality healthcare for underserved populations.
What causes cervical cancer?
High-risk human papillomavirus (HR-HPV) is likely a primary cause of about 91 percent of all cervical cancers in the U.S., according to the Centers for Disease Control and Prevention (CDC).
About 9 in 10 HPV cases dissipate on their own within two years, according to the CDC. But when a case doesn't, it can cause genital warts or cancer—sometimes years or even decades later.
HR-HPV alone doesn't cause cervical cancer but does when other risk factors, such as tobacco use, immune suppression, stress or poor nutrition, are present, according to Judith Smith, Pharm.D., a professor in the McGovern Medical School Department of Obstetrics, Gynecology and Reproductive Sciences at UTHealth Houston
Why are late-stage cervical cancer rates increasing?
The new study was observational, so it couldn't identify why advanced-stage cervical cancer is becoming more prevalent, but the overall rate of cervical cancer has increased slightly since 2000, according to the ACS. Factors including vaccine hesitancy and access limitations, missed screenings and lack of education could be to blame.
"Any increase in cervical cancer is concerning. We have seen a sharp increase in overdue screenings in women, which could be leading to missed opportunities to find precancerous lesions and prevent disease progression," said Kameelah Phillips, M.D., an OB-GYN, a women's health expert and the founder of Calla Women's Health in New York City.
Phillips and Smith added that early-stage cervical cancer is often asymptomatic, and many women might not know the early signs and symptoms of advanced cervical cancer. These include unusual vaginal bleeding, including after intercourse or between periods; watery, bloody, often foul-smelling vaginal discharge; and pelvic pain.
"Another problem is [the] inherent, common trait of women to worry about taking care of everyone else in their lives—children, parents, family, etcetera—and ignoring [or] putting off the warning signs until the pain or bleeding gets disruptive to their daily routine, tasks [and] responsibilities," Smith said.
The disease also disproportionately affects non-white populations, especially Black women, something the study authors noted is consistent with a broader trend in health and healthcare inequities. The study indicates 1.55 per 100,000 Black women were diagnosed with distant-stage cervical cancer, compared with 0.92 per 100,000 white women.
"Like many other areas of healthcare, racial and ethnic inequities significantly exacerbate the impact of cervical cancer on Black and Hispanic women," Phillips said. "Studies have found Black women are twice as likely to die from cervical cancer than white women for reasons including a lack of access to insurance and appropriate treatment.
"Other challenges that affect a woman's access to healthcare can include transportation, health literacy and trust in their healthcare provider," Phillips continued. "Many women believe they will experience financial barriers to screening that they're unable to overcome, particularly related to screening appointment costs and potential follow-up or future treatment costs. These findings highlight the importance to continue to improve screening access."
Despite significantly higher rates of cervical cancer among non-white populations, the study found late-stage cervical cancer rates increased most significantly among white women: at a rate of 1.69 percent, compared with 0.67 percent for Black women. White women in the South ages 40 to 44 had the highest rate of all, at 4.5 percent, followed by 30- to 34-year-olds.
At the same time, the findings indicate white women were nearly twice as likely to have missed screenings: 26.6 percent compared with 13.6 percent of Black women. And white teens ages 13 to 17 years had the lowest HPV vaccination rate. The reasons are unclear. Previous studies suggest white parents were more likely to express biases against the HPV vaccines and concerns about its safety, but Smith said it is not safe to extrapolate between studies.
"I often hear concerns about vaccine safety and concerns that it will make their children sexually active before they are ready. This is certainly not the case, and vaccine safety has been well established," Phillips said. "There is also a serious misconception that this vaccine is only for female children. I reiterate to all of my patients that the HPV vaccine is not only very safe but highly effective."
Phillips and Wendy Goodall McDonald, M.D., an OB-GYN at Women's Health Consulting and Northwestern Medicine Prentice Women's Hospital in Chicago, said a lack of vaccinations in those over-30s could factor in as well. Goodall McDonald noted that people in their early to mid-30s were among the first to be offered the original HPV vaccine. At the time, there was a lack of awareness and a fair amount of hesitation, which might have led many people to forgo vaccinations.
Cervical cancer prevention
Smith, Goodall McDonald and Phillips said a combination of HPV vaccination and testing and routine Pap smears are the best means of prevention against cervical cancer. Importantly, HPV vaccination and testing alone are not always sufficient. Routine Pap smears are essential regardless of vaccination status because HPV tests don't always indicate when cancer is present.
The HPV vaccine is one of the safest and most effective vaccines in existence, according to the American College of Obstetricians and Gynecologists (ACOG). When administered to people who haven't been exposed to HPV, its efficacy rate is more than 99 percent. Besides protecting against cervical cancer, it can also reduce the risk of other HPV-related cancers, including anal cancer, rectal cancer, head and neck cancers, penile cancer and vaginal/vulvar cancers. ACOG recommends people get the HPV vaccine in early adolescence, around age 11 or 12, though the vaccine can be administered as early as age 9.
"The earlier a person gets vaccinated, the less likely they are to contract certain aggressive strains of HPV. Once a person is exposed to HPV through intercourse, the amount of protection reduces," Goodall McDonald said. "Male partners can't be screened for HPV, so it's hard to completely protect yourself from the virus apart from the use of condoms. It is best to get vaccinated prior to any HPV exposure, but a person can still benefit from HPV vaccination until the age of 45. That applies to all people: men, women and nonbinary people."
The frequency of testing for cervical cancer and HPV depends on a person's age and risk factors, such as a history of HPV or abnormal Pap results. But ACOG recommends most women begin cervical cancer testing by age 21.
Goodall McDonald stressed the importance of safe sex as well.
"Condom and barrier use can help reduce the spread of HPV. Not sharing or properly cleaning sexual toys is also important for HPV and other STI prevention," she said. "HPV can also be transmitted orally and is a cause for oral, throat and anal cancer, so barriers should ideally be used in all sexual circumstances."