How Are Varicoceles Diagnosed and Treated?

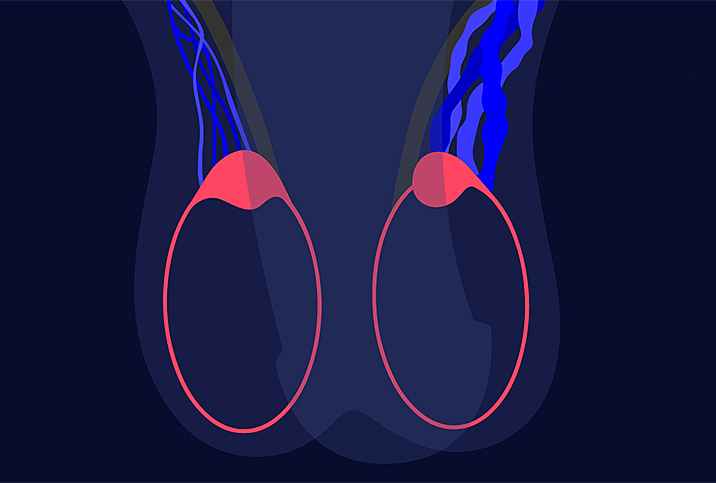
A varicocele is the swelling of the veins in the scrotum above the testicles. It's a relatively common condition, affecting some 10 percent to 15 percent of adult men at some point in their lives, as well as 20 percent of adolescent boys.
As the name suggests, varicoceles are related to varicose veins—the swelling of veins in the legs.
Varicoceles aren't typically life-threatening and usually cause only mild symptoms or even no symptoms at all. They are known to be a cause of infertility, however, and may cause other issues if they occur during adolescence.
How are varicoceles diagnosed?
Diagnosing varicoceles usually begins with a physical exam during which a healthcare provider palpates the area above the testicles within the scrotal sac.
Higher-grade varicoceles are often apparent to the naked eye. They have often been described as resembling "a bag of worms" or spaghetti inside the scrotum above the testicles because the veins become so swollen and pronounced.
Your healthcare provider may ask you to perform the Valsalva maneuver, a physical, drug-free test that's used to restore a person's heart rate to normal as well as to diagnose venous diseases.
To perform the maneuver, stand up and try to push the air out of your lungs while keeping your mouth and nose shut. While you're doing that, your doctor will feel for any changes in your scrotal veins.
A varicocele is a common, non-life-threatening condition that many men may not even know they have. It may not require any medical intervention.
Other tests may include the following:
- Blood test. There may be a blood draw to analyze testosterone levels and other hormone levels.
- Pelvic ultrasound. This non-invasive imaging test gives your healthcare provider a more precise view of your scrotal veins to ensure there is no testicular torsion. This is when the spermatic cord rotates, becomes twisted and cuts off the blood supply to a testicle, which is an emergency condition that requires immediate treatment.
- Semen analysis. If there's a question of a varicocele affecting your fertility, your doctor may suggest a semen analysis.
Once the tests have been evaluated, your varicocele will be graded:
- Grade 0. The smallest type of varicocele, it can be felt during a physical exam but can only be seen on ultrasound.
- Grade 1. The varicocele isn't visible, but your doctor will be able to feel its presence when you perform the Valsalva maneuver.
- Grade 2. Your doctor can feel the varicocele even when you're not performing the Valsalva maneuver, but it still isn't visible.
- Grade 3. This is the most pronounced varicocele, visible to the naked eye.
How are varicoceles treated?
The recommended treatments for a varicocele range from doing nothing at all to various types of surgical interventions, depending on the grade of the varicocele.
If it isn't causing you any discomfort or fertility issues, you may elect to leave it alone. If you sometimes have discomfort, a simple solution is to wear tighter-fitting underwear while you're doing physical activities or if you're on your feet for long periods of time.
For many patients, ice or cold packs can help relieve symptoms and discomfort, while others may need to add over-the-counter pain relievers, such as ibuprofen, to their routine.
If your healthcare provider suggests more action is needed, the next step may be a varicocelectomy. This is a set of surgical procedures for treating severe varicoceles that are causing discomfort, affecting fertility or affecting adolescent development. As part of a varicocelectomy, the urologist will cut the affected veins and seal them off, re-routing the blood flow to other veins.
"There's the microscopic subinguinal varicocelectomy or microscopic inguinal varicocelectomy. Those are the most effective, least chance of complications, least chance of recurrence," said Neel Parekh, M.D., a men's fertility and sexual health specialist with Cleveland Clinic.
If a microsurgical varicocelectomy is being carried out because the patient is in pain, the inguinal approach is often used. This allows access to the ilioinguinal nerve that can be cut to provide relief.
The incision for inguinal surgery is made a little higher in the groin than the incision for a subinguinal varicocelectomy. The surgery lasts about 30 to 60 minutes and is typically performed as an outpatient procedure. A return to full activity may take as long as three weeks, but most men are up and about within 72 hours.
"I perform a microscopic subinguinal varicocelectomy," Parekh said. "Then there's open surgery—that's not done in the United States that often—where they have it done not using a microscope but an inguinal incision. Then you have the laparoscopic approach—that's typically done in the adolescent/pediatric population—and the percutaneous embolization procedure. That's a procedure where they place a coil in the testicular vein to fix the varicocele."
A laparoscopic varicocelectomy is performed by passing surgical tools through small incisions in the lower abdomen, with all the action monitored by a video camera. The network of veins above the groin is less complex, so the procedure is easier to navigate.
What problems are associated with varicoceles?
Varicoceles are generally harmless and frequently don't require treatment if they're not bothersome. They can, however, affect other issues, including fertility, testicle development and testosterone production.
How varicoceles can affect fertility
While the evidence is inconclusive that varicoceles cause male infertility, they are considered to be associated with lower fertility, according to the World Health Organization (WHO). Indeed, 4 out of 10 men who are tested for fertility problems have a varicocele. One hypothesis is that having that extra blood pooling near the testicle may affect its ability to produce sperm.
"The testicles sit in the scrotum so they can be two to three degrees Celsius cooler than your core body temperature," Parekh said. "So the theory on how varicoceles affect fertility is that the veins raise the temperature of the testicles, which doesn't make it a good environment for sperm production."
For many guys, semen parameters improve a few months after surgical varicocele repair.
How varicoceles can affect testicle development
Varicoceles may potentially slow the development of an adolescent's testicles, or at least contribute. Frequently, a higher-grade varicocele in a teenager may be associated with one testicle being less developed than the other.
If the varicocele is detected early enough, surgical intervention can allow the affected testicle's growth to catch up.
How varicoceles can affect testosterone production
Varicoceles may be associated with lower testosterone production. Just as the excess blood near the testicle may affect its ability to manufacture sperm, it can impede testosterone production.
How varicoceles can cause discomfort
Some larger varicoceles can cause discomfort and even pain that's severe enough to affect a man's quality of life. Even if they don't have fertility concerns, having a surgical intervention may be the best option for these men.
What's the outlook if I have varicoceles?
Some 3 million men per year are diagnosed with varicoceles, so it's a common condition. It's one that many men live with without knowing they have it.
Even for guys who have fertility concerns or other reasons to seek surgical intervention, the prognosis for varicoceles is positive. Within two years of having varicocele repair surgery, there was a significant increase in motile sperm production as well as spontaneous pregnancy, according to a 2002 study.
A 2017 meta-analysis of adolescents who had varicocele surgery indicated there was a significant increase in both testosterone production and testicular volume (the size of the previously affected testicle).
The bottom line
A varicocele is a common, non-life-threatening condition that many men may not even know they have. It may not require any medical intervention.
If surgical treatment is required, the outlook is usually a positive one, recovery is fast, and you can look forward to living a full and pain-free life with improved fertility and increased testosterone production.