There Are Microsurgical Options for Varicocele Treatment

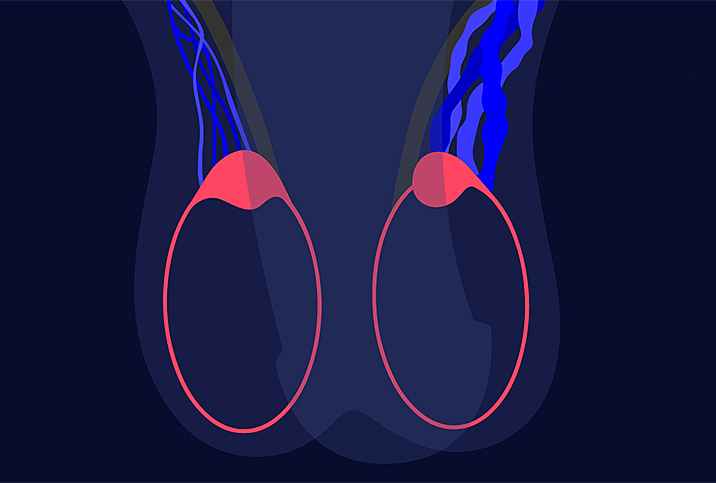
A varicocele is an enlargement of the veins in the scrotum, the bag of loose skin that holds the testicles. Ordinarily, the scrotal veins carry blood lacking in oxygen from the testes. In cases of a varicocele, however, blood pools in the testicular veins instead of circulating away from the scrotum.
This condition usually occurs during puberty and either improves or worsens as the patient ages. While varicoceles can be uncomfortable or even painful, they do not usually have serious complications.
However, a varicocele can cause the poor development of a testicle, low sperm production or other problems that may lead to male infertility. A 2017 study cited estimates of varicoceles affecting 15 percent to 20 percent of the male population. More than 40 percent of males diagnosed with infertility owe that diagnosis to a varicocele.
But the same study also stated varicoceles are the most correctable cause of infertility, and there are multiple options for treating them, including microsurgery.
What is microsurgery?
Microsurgery is a specialized discipline that uses compound microscopes and miniaturized instruments to operate on small and delicate structures 1 millimeter or less in diameter. It is also used to operate on sensitive organ systems, including blood vessels and nerves.
This procedure is commonly used for complicated reconstructions of skin, muscles and tissues. For the most part, different techniques within the discipline are used to graft or repair nerves or damaged blood vessels and can also be used for vascular grafting and the transfer of free tissue.
Microscopic varicocelectomy is an effective treatment option for men with scrotal pain, infertility and low testosterone caused by scrotal varicoceles, according to Alex Shteynshlyuger, M.D., a urologist at New York Urology Specialists in Brooklyn.
"Microscopic varicocelectomy is a gold standard with the greatest success rate and lowest rates of complications," he explained. "It is often performed for patients who underwent unsuccessful embolization."
Who is a candidate for varicocele treatment?
Varicoceles affect men of all ages. The American Urological Association (AUA) recommends treatment for male partners in a couple trying to conceive, provided they meet the following conditions:
- A palpable varicocele
- Documented infertility
- The female partner's cause of infertility is treatable
- The male partner has abnormal sperm functions or semen parameters
For adult males who are not trying to father a child, varicocele repair or treatment is also recommended if they have a palpable varicocele and abnormal semen parameters. Urologists also recommend treatment for adolescent males with a varicocele and reduced testis size.
Microsurgery vs. laparoscopic surgery
Laparoscopic varicocelectomies are performed on patients whose symptoms are relatively minor. These procedures involve an incision in the lower abdomen as opposed to the groin, which is the access point for microsurgery. Surgeons can perform this procedure in as little as 30 minutes because fewer veins need to be ligated, or tied off.
Microsurgery is recommended for patients with more severe symptoms, particularly deep-seated pain, because the swelling is deeper within the scrotal area, according to Justin Houman, M.D., a reproductive urologist and men's health specialist at Tower Urology in Los Angeles and the medical director for Bastion Health, an app-based telehealth platform for men. On average, a microsurgical procedure for a varicocele can run from two to four hours.
Regardless of the procedure, surgery within the scrotal area poses the following risks:
- A hydrocele, or a buildup of fluid around the testicles
- Recurrent venous swelling (repeat varicocele)
- Postsurgical infection
- Arterial damage
- Chronic testicular pain
- Hematoma, or blood pooling around the affected testicle
Options for varicocele microsurgery
Two types of microsurgical procedures are considered for treating varicoceles: inguinal and subinguinal. The terms refer to the part of the groin in which surgeons make the necessary incisions.
Inguinal varicocelectomy
The contemporary approach to inguinal microsurgery involves making a 3- to 5-centimeter incision over the inguinal canal, Houman explained. The inguinal canal is a passage in the lower anterior abdominal wall.
The surgeon then opens the external oblique aponeurosis to deliver the spermatic cord. The cord is then lifted out, and any external spermatic veins running parallel to it or perforating the floor of the inguinal canal are identified and ligated. Afterward, internal spermatic veins are identified under a compound microscope, dissected and ligated with sutures or surgical clips.
In the case of inguinal procedures, the vas deferens, vasal vessels, lymphatic channels and testicular artery are left intact. Following the operation, testicular venous return (blood flow) goes through the vasal veins, which in turn drain into the internal pudendal system.
Subinguinal varicocelectomy
In a subinguinal varicocelectomy, the incision is made just over the top of the penis. Some surgeons need to make two incisions over the inguinal canal to extract the spermatic cord and expose the affected veins in the scrotum.
Shteynshlyuger considers the subinguinal approach less invasive but nevertheless effective. He explained that semen quality improves in patients who undergo this form of microsurgery, and scrotal discomfort and morbidity are also minimal.
Microscopic subinguinal varicocelectomy has a shorter recovery period, allows for a smaller incision and gives access to all the varicose veins that need to be addressed, Shteynshlyuger added.
Following a successful varicocelectomy, patients can return to their jobs in one to three days. Most even go home the same day. However, strenuous activities such as climbing ladders, sports and heavy lifting should be avoided during the first week following varicocele surgery to avoid complications. On average, full recovery takes at least two to three weeks.
Follow-up physical exams are necessary within two weeks of surgery to make sure the wounds are healing properly.