Urinary Issues Could Point to One of Two Prostate Conditions
Sometimes it seems as if the prostate gland is a biologically variant time bomb designed to go off randomly, complete with devastating effects which create a plethora of potentially difficult scenarios for men older than age 50.
Of course, there's prostate cancer. Then there's the potential for developing a weak prostate or experiencing prostate-related erectile dysfunction (ED). Finally, you have two conditions that both involve inflammation of the prostate, which can manifest for different reasons with different (but similar) presentation qualities.
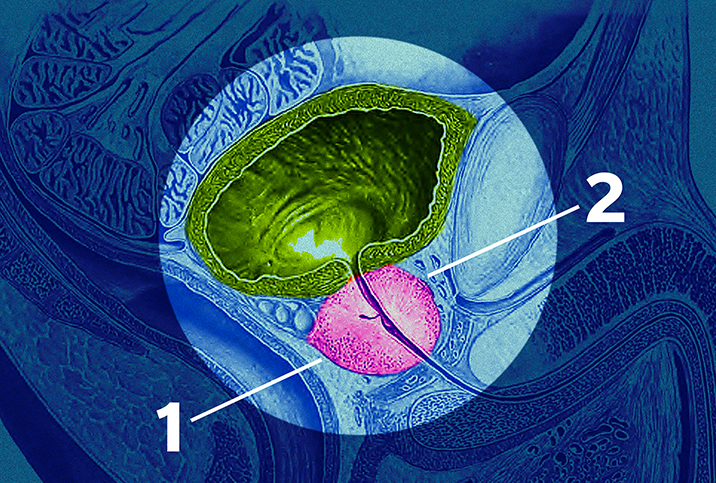
Prostatitis and benign prostatic hyperplasia (BPH) both affect the way men urinate, so it's important for you and your doctor to be able to tell the two apart by taking into account your symptoms and medical history.
BPH vs. prostatitis basics
BPH is an enlargement of the prostate that occurs commonly as people age, often after age 50. When it grows too much, it can cause bladder outlet obstructions.
"[Patients] tend to present with poor flow intermittency, so when they pee, it's not a continuous flow," said Wael Almajed, M.D., a urologist and sexual medicine specialist on fellowship with Tulane University in New Orleans. "They kind of pee and then stop and pee again and try to strain to get the urine out. And also, they may have some hesitancy, which is sometimes they go to the toilet and they want to pee but it takes them time to initiate the stream."
Put simply, when the prostate is enlarged, some men can't push the urine through because of an obstruction.
"BPH can have more of an insidious, gradual onset," said Matthew J. Mutter, M.D., an assistant professor of clinical urology at the Louisiana State University School of Medicine. "Prostatitis is more like you wake up in the morning and you begin having symptoms. So from that standpoint, they are a little different, and that's one of the things we would look at in the evaluation of a man who comes in with prostate issues."
In other words, BPH could affect functionality a bit more harshly when untreated, though both conditions can cause discomfort, pain and other complications. Where BPH's symptoms are obstructive in nature, prostatitis's symptoms would more likely be classified as irritative, Mutter said.
However, there can be a lot of gray area in between how the two conditions manifest and present themselves.
Symptom similarities and differences
"With BPH, a lot of times [patients] come with what are called voiding symptoms, and voiding symptoms are basically symptoms that are related to the obstruction," Almajed said. "So they tend to have poor flow, hesitancy and intermittency, and a feeling of incomplete emptying."
With prostatitis, which is an infection and not just inflammation, men tend to experience storage symptoms that are the opposite of voiding symptoms.
"They have to go to the toilet very often," Almajed said. "They don't have any issue with the flow of the urine, but sometimes they have burning urination. They tend to have frequency and urgency, so when they have to pee, they can't hold it and they have to go right away. And also, during the night, sometimes they wake up multiple times to urinate. And they may have pelvic pain or burning during urination."
How much urination is too much urination? Almajed offered some general rules and habit-based considerations.
"In general, we expect men to pee regularly between four to six times a day," he said. "And in general, we expect [adults] to not wake up at all during the night [to urinate]. Obviously, it depends on oral intake, so if someone is always drinking water throughout the day, they may go more frequently to the toilet. But it's also the sensation that the patient can't hold the urine, the urgency."
If the frequency of your urination pattern doesn't coincide with your hydration habits, but you still experience the severe urge to use the restroom, it's possible this experience is tied to an inflammation of the prostate in one way or another.
Patients suffering from prostate inflammation like that associated with BPH and/or prostatitis may urinate as much as every half-hour or more, even if not much urine comes out each time. The issue is not that their bladder becomes full more quickly, but rather that they can't store it correctly because of the irritation. Remember that irritative symptoms are more commonly associated with prostatitis but can be evident in cases of either condition.
Fortunately, doctors can determine what they are dealing with through further evaluations.
Evaluations and examinations
BPH and prostatitis sometimes have similar symptoms. To differentiate them, doctors take a detailed history and likely perform a digital rectal exam (DRE).
"If it's BPH, the prostate is found to be enlarged but in general it's not tender on examination," Almajed said. "While in prostatitis, the prostate tends to be tender, so when we feel for the prostate, the patient will get extreme pain from it."
In addition to urinalysis and other typical urological lab work, your doctor also has unique tools available for further analysis.
"We do express prostatitis secretions, which means that while we're examining the prostate, we kind of try to push on the prostate and will push prostatic fluid through the urethra," Almajed said. "And we look at it under the microscope and sometimes we culture the fluid, as well, looking for bacteria or anything that can cause prostatitis."
Once doctors have determined which condition is in play, the course of action may become clear or the patient may begin a long-term—perhaps even lifelong—dance with their prostate's health and overall condition.
Treating either condition
"Prostatitis will have sort of flare-ups, where you can treat a flare-up and, generally speaking, things will resolve," Mutter said. "BPH is more of a chronic condition or more of a condition of an older man. While it's treatable, BPH is going to ultimately cause more issues when it's untreated than prostatitis. Ultimately, BPH will affect your ability to empty your bladder, and if you can't empty your bladder, then you can start to have upstream effects, kidney issues. It could be more serious in the long term."
Acute prostatitis can be treated with antibiotics and anti-inflammatory medications. Chronic prostatitis may be more complicated and can manifest in multiple different forms, which are some of the most common cases of prostatitis doctors see, and the approach may be very symptom-focused. Doctors can make recommendations involving activity or water intake to alleviate certain aspects of the symptoms patients feel, and medications may be available to prevent symptoms from generating additional consequences. Patients might fill out a questionnaire to help determine which symptoms deserve the highest priority in their medical plan.
Patients are also advised to generally avoid beverages associated with frequent urination, such as sodas or caffeinated drinks. Other lifestyle alterations doctors might recommend—what's good for the heart is good for the prostate—should benefit patients from a whole-body perspective while improving symptoms.
A lot of times, medications for these conditions need to be taken for life, so patients may desire to pursue alternative options, including surgery, to prevent the issue from worsening or remaining stagnant without remedy.