Get to Know the Types of Cervical Precancers & Cancers
A diagnosis of cervical precancer sounds to many women like the end is near, but you shouldn't let that fear hang over you, because such a diagnosis is much less likely than it used to be.
Anatomy of cervical cancer
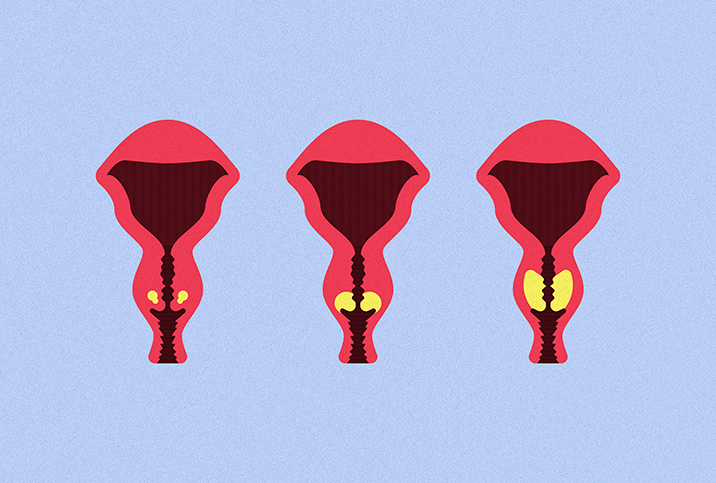
We tend to think of the cervix as one homogeneous area, but it’s slightly more complicated than that. Understanding the varieties of cervical tissue and the locations where cancerous cells can grow will help you understand the types of cervical cancers.
The cervix consists of two areas: the endocervix and the exocervix, also known as the ectocervix, which is what is visible to a doctor during a pelvic exam. The endocervix, or inner portion, is covered in glandular cells; the exocervix, or lower portion, is covered with stratified squamous cells. Each of these sections can grow abnormal cells that can become cancer.
There is also a third location called the transformation zone, which is where the endocervix and exocervix overlap. This area contains both glandular and squamous cells, and it is where most forms of precancer begin and where your doctor will take cells during a Pap smear.
Precancer of the cervix
Following a Pap smear, your doctor will send the cell samples to a lab, and the results will come back one of three ways: normal, unsatisfactory and abnormal.
An abnormal Pap smear is the result women dread. However, “abnormal” is often no more than an indication of a precancerous condition, and the odds are better than you might think: Only about 1 in 10 abnormal Pap smears may turn into cervical cancer.
With an abnormal result, the cells in question are identified as either squamous (external) or glandular (internal) cells. Then, the cells are classified based on multiple grades, such as atypical, low-grade and high-grade, which will determine your doctor’s treatment plan.
These three classifications typically result in repeated Pap smears and a wait-and-see approach. Often, a poor test sample is the problem, and a repeated test can rule out precancerous conditions.
An adenocarcinoma in situ result indicates a precancerous condition, usually a lesion on the cervix. The most common treatment plans involve burning off the lesion or removing part of the cervix to stop the lesion from spreading.
Without treatment, precancerous cervical cells can turn into cervical cancer. Luckily, with treatment, most precancerous conditions never get the chance to turn into cancer, which is why routine Pap smears are so important. Guidelines vary, but the U.S. Preventive Services Task Force recommends Pap tests every three to five years for most women between the ages of 21 and 65.
Types of cervical cancers
Cervical cancer was once the leading cause of cancer death in women, but this is no longer true. With early detection, most women beat it.
The two main types of cervical cancer are squamous cell carcinoma and adenocarcinoma. Squamous cell carcinoma is a cancer of the external tissue of the cervix, and it is the most common form of cervical cancer. Treatment often involves removing part or all of the cervix. Depending on your family history with cancer and the size of the cancerous lesion, your doctor may recommend a hysterectomy.
Adenocarcinoma is a more aggressive form of cervical cancer that can advance quickly and is resistant to most radiation therapies. While this diagnosis does not automatically mean a dire prognosis, it does mean that your doctor will likely recommend a full hysterectomy and aggressive chemotherapy.
Regardless of the type of cancer, the most important diagnostic element is determining the stage of cancer. Your doctor will perform examinations to identify the location and size of the cancerous lesion and will perform a biopsy and other lab tests to determine your cancer stage.
Stage I is the most common diagnosis of cervical cancer and provides the best prognosis because the cancerous cells are isolated to the cervix and haven't spread to the uterus or other nearby organs. Removal of the cancerous region is the usual recommendation, combined with a round of either chemotherapy or radiation, depending on the type of cancer.
If your doctor determines you have stage II, III or IV, your cancer has likely been present for some time and has spread to other parts of your body. While these stages are more difficult to treat, it is still possible to overcome this diagnosis.
Living with cervical cancer
The detection and treatment of cervical cancer have advanced significantly in the past 30 years. As a result, most cervical cancers that are caught in the precancerous stages are treated and eliminated before they turn into cancer. While most of us would prefer not to have to think about cancer at all, the truth about cervical cancer is that regular screenings can prevent it.