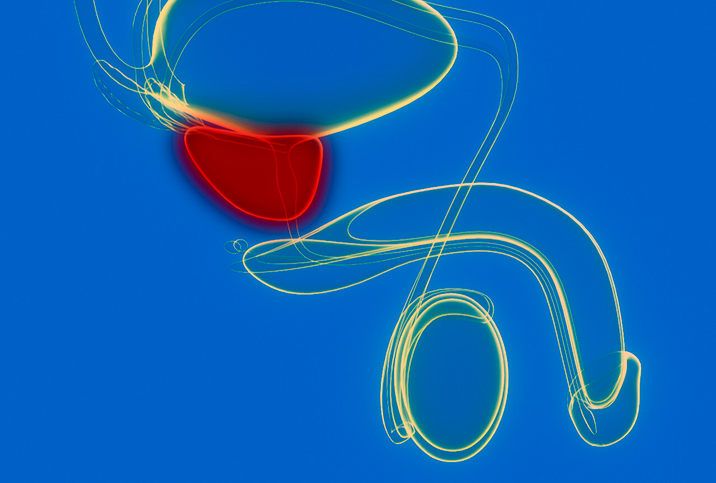
Prostate Cancer: Myths & Misconceptions
As a man ages, his chance of developing prostate cancer grows exponentially. About 1 in 8 men will be diagnosed with the disease during his lifetime, with some 60 percent of those cases occurring in men age 65 or older.
The misconceptions about prostate cancer are as widespread as the disease itself, and while many have surfaced as a means to manage fear, these myths can often do more harm than good. To stay safe, it's best to know the truth.
Myth: Prostate cancer always causes symptoms.
Reality: Prostate cancer rarely shows symptoms until it is in an advanced stage. While other prostate complications, such as urinary difficulty, might prompt a doctor visit, cancer symptoms such as bone pain and pelvic pain occur only after cancer has spread to different parts of the body.
Screening for prostate cancer is done with a digital rectal exam (DRE) or a prostate-specific antigen (PSA) test. If either is abnormal, it might prompt a biopsy. Most prostate biopsies are transrectal ultrasound-guided.
Myth: If I have no family history of prostate cancer, I won't get it.
Reality: While family history is certainly one risk factor, developing prostate cancer doesn't always come down to genetics. Many men with no history of prostate cancer in their family are diagnosed with prostate cancer, and many men with prostate cancer in their family never get it.
Myth: Elevated PSA levels indicate prostate cancer.
Reality: While the prostate-specific antigen (PSA) test is a useful tool in diagnosing prostate cancer, it's by no means conclusive. Prostate cancer does produce some PSAs, but so does a healthy prostate gland. Higher PSA levels can also result from:
- Recent ejaculation
- Riding a bicycle
- Noncancerous enlarged prostate
- Prostatitis (inflamed prostate)
- The digital rectal exam itself
If your PSA test shows elevated results, your doctor will almost certainly ask you to come back to be retested. A second test with high prostate-specific antigen levels may lead to further evaluation with a prostate biopsy. The bottom line is that the PSA is just one of an array of tests that give you and your doctor information about your prostate. On its own, the prostate-specific antigen test is not a conclusive diagnostic tool.
Myth: All prostate cancers are deadly.
Reality: There are different grades of prostate cancer, meaning different levels of aggressiveness. Some cancers need treatment; some can be safely observed. After a biopsy confirms the presence of cancerous cells in a man's prostate, a diagnosis by a pathologist will determine which type is present and how aggressive it's likely to be.
Several factors affect the decision for treatment, including the extent and aggressiveness of the cancer, as well as the age, health, life expectancy and preferences of the patient. Men should know that prostate cancer is a complex, multifaceted disease for which there are multiple treatment options. Active surveillance, which is monitoring the prostate, is a common management strategy for less aggressive tumors.
Myth: Prostate cancer diagnosis means treatment must start immediately.
Reality: Surprisingly, one of the treatments that clinicians consider for prostate cancer is to do nothing. Many types are slow-growing and don't spread, and aggressive interventions would be more harmful than the disease itself.
The Gleason score is a description by pathologists about the aggressiveness of cancer. Tumors are graded 1-5 based on their patterns under the microscope. The two most prevalent patterns are added together, so the least aggressive score would be 1+1 = 2 and the most aggressive would be 5+5=10. In general, a Gleason score of 6 or less is considered "low grade," and the cancer is generally not treated. Gleason 7 is "intermediate" and Gleason 8-10 is "high grade."
Several professional clinical societies—including the American Society of Clinical Oncology, the National Comprehensive Care Network and the American Urological Association—recommend active surveillance as an appropriate approach for prostate cancers rated Gleason 6 and lower.
Myth: Prostate cancer surgery means the end of my sex life.
Reality: Your sex life after prostate cancer won't be over, but it will be affected. The nerves that control erections are alongside the prostate and are often affected by cancer surgery. Depending on the location and extent of the cancer, surgeons may perform a "nerve-sparing" technique to reduce the injury to the nerves. Even with the best techniques, erections will often suffer after surgery. There is usually some improvement with time, and younger men tend to have quicker recovery. After surgery, a man may need to use additional therapies, such as pills, constriction devices, injections or even a penile prosthesis, to help with erections.
Prostate cancer is serious, but may not be as scary as you think. Testing and treatment are more advanced and the disease more understood than ever before, so don't let fear and misunderstanding keep you from your best health.