Online Birth Control Options Increase Access, But Barriers Still Exist
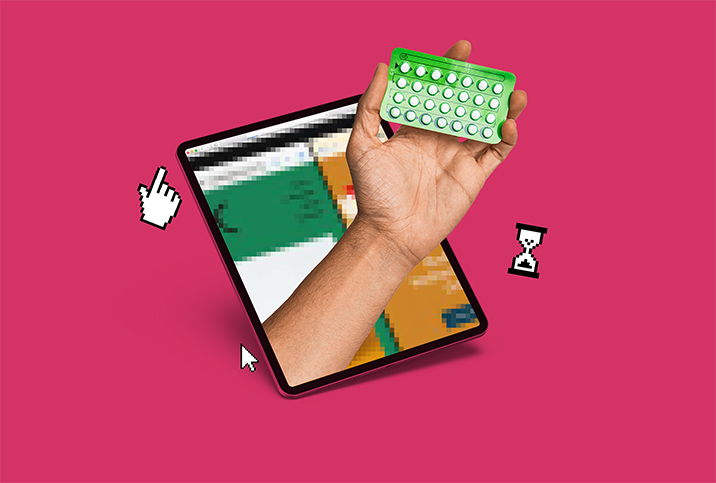
While scrolling on social media, you've probably stumbled upon ads for birth control companies describing hassle-free and cheap options that deliver prescriptions right to your door.
Since 2019, the use of telehealth has increased, with 95 percent of health centers using online services during the COVID-19 pandemic. The use of telemedicine allows patients to receive care from their homes—and physicians to lower the costs of visits and treat patients in a wider geographical area.
This expansion includes online contraceptives. Companies have helped many individuals receive care for sexual and reproductive health by providing low-cost or free medication with discreet shipping.
However, according to a 2020 survey from Kaiser Family Foundation, 18 percent of women are not using their preferred method of contraception, and 25 percent say it's because they can't afford it. Health insurance coverage—or lack thereof—is often a deciding factor.
In-person care vs. telehealth
The Affordable Care Act (ACA) was enacted in 2010 to lower the costs of health care, including mammograms, screenings, prenatal care and other services—such as contraceptives. The Women's Preventive Services Guidelines state that covered contraceptives include intrauterine devices (IUDs), condoms, patches, rings, and injectable and oral contraceptives.
With an estimated 88.2 percent of women ages 15 to 44 using at least one form of contraception in their lifetime, telehealth options have allowed for increased accessibility. Prescriptions are delivered through apps or websites for free or through low-cost consultations and plans.
Telehealth and online contraceptive options have given individuals accessibility regardless of insurance, financial issues, location and transportation. However, insurance remains a deciding factor on costs and types of birth control available.
Additionally, telehealth does not entirely replace in-person visits. About 53 percent of individuals still prefer an in-person visit, according to post-pandemic patient preferences highlighted in a 2021 assessment published in the Journal of the American Medical Association (JAMA). However, 23.5 percent of individuals switched to telehealth services when confronted with higher costs of in-person care.
Nurx, SimpleHealth, the Pill Club and Wisp are examples of personalized telehealth services that use physicians and industry experts to provide medical expertise remotely. Each company delivers different forms of birth control with discreet packaging, free shipping and automatic refills. Patients receive online consultations with licensed providers to request a prescription and determine what birth control fits their health profile.
San Francisco-based Nurx provides more than 50 birth control formulas, including the pill, patch, ring and shot. Additional prescriptions are available for skin care, migraines, PrEP and herpes, and home tests are available for sexually transmitted infections (STIs), human papillomavirus (HPV) and COVID-19.
SimpleHealth and the Pill Club offer more than 120 generic and name-brand birth control options. The companies also provide period care, supplements and other protective services. Wisp offers birth control options, emergency contraceptives, intimate care and COVID-19 testing.
Nurx's chief medical officer, Nancy Shannon, M.D., Ph.D., said telehealth has revolutionized accessibility for sexual and reproductive health care.
"Unfortunately, there is still stigma and shame surrounding sexual health preventing people from getting the care they need," Shannon said. "We hear so many stories about people's doctors shaming them for asking for birth control, saying, 'You're not married, why do you need this?' or 'You're married, why don't you want a baby?'"
Thankfully, low-cost options are available
Following implementation of the ACA, the average out-of-pocket spending on birth control decreased. Individuals saved, on average, $248 for IUDs and $255 annually for contraceptive pills, according to a 2015 data analysis published in the journal Health Affairs.
Although out-of-pocket spending has decreased, online birth control services depend on insurance for copay and consultation and to determine the type of birth control available to a patient.
"We bill insurance, and many options have a $0 copay with insurance," Shannon said. "It depends on your plan which options are free, but most insurance plans are required by law to offer some form of birth control for a $0 copay. For those without insurance, we offer popular pills for $15 per month, both a combination pill [containing estrogen and progestin] and a progestin-only pill."
New York-based SimpleHealth provides a monthly plan with a similar copay structure.
"The medication itself is typically $0 out-of-pocket for those with insurance and starts at $7 a month for those without insurance," said Alliccia Odeyemi, M.S., director of public relations and partnerships at SimpleHealth.
Although SimpleHealth provides a $0 copay, the company charges a $15 consultation fee for people without insurance.
Similarly, the Pill Club charges $15 for a consultation without insurance but a free consultation with insurance. Birth control starts at $6.99 per month or $15 a year for online consultation and prescription.
Wisp starts at $5 a month with a free consultation. Additionally, members receive their first month supply free. Compared to other online birth control services, Wisp is not covered by insurance. However, prescriptions can be transferred to a pharmacy to be covered.
The importance of accessibility
Although telehealth has reached individuals around the country, many companies do not offer online birth control in every state. Nurx provides birth control home delivery services to 36 states, SimpleHealth to 32 states, and the Pill Club and Wisp to all 50 states.
Additionally, insurance is a deciding factor on what types of birth control are available for patients.
"Many women find barriers to obtaining birth control can include lack of insurance, cost, difficulty obtaining an appointment or access to a clinic or physician," said Mia Mowzoon, M.D., an OB-GYN at Northwell Health in New York City.
According to Mowzoon, of 1,385 women surveyed in a 2016 study, 29 percent reported they tried to obtain a prescription for hormonal contraception but had problems accessing the initial prescription or refills.
Despite the availability of online consultations, Mowzoon indicated that telehealth should not substitute for in-person visits.
"All women should talk with their gynecologist about the best option for their body, which requires an in-office visit," Mowzoon advised. "Downsides of online appointments and increased virtual accessibility to birth control are that women are visiting their gynecologist less frequently."
Mowzoon added that breast examinations, cervical cancer screening and STI screening are all important preventive health screenings that should not be missed and must be conducted in person.