Hormonal versus Copper IUDs
You probably wouldn't think IUDs have much in common with a famous rotisserie chicken infomercial, but one phrase is true for both of them: Set it and forget it.
Once inserted, IUDs are effective for anywhere between 5 and 12 years, there's nothing you need to remember to do daily, and studies show they are more effective than the birth control pill (they are more than 99 percent effective in preventing unplanned pregnancies).
It's for these good reasons that IUDs are growing in popularity—for context, in the mid-'90s, when this type of birth control was relatively new (the copper IUD debuted in 1988), just 1.5 percent of women who used contraception had one; by 2013 the percentage had risen to just under 10 percent and by 2017 that number had jumped to 14 percent.
"IUDs are my favorite form of contraception. They are long-acting and reversible immediately upon removal," Nichole Butler, M.D., board-certified OB-GYN, F.A.C.O.G., said.
However, once you decide to get an IUD there's still one more decision to make: hormonal or copper? Here we spoke with Butler and women with both types of IUDs about the pros and cons of each.
Hormonal IUDs
"I found my IUD to be a breeze. I like it enough that I'm now on round two of the same brand [Liletta]. I've been lucky enough not to have any side effects, other than the convenience of not having a period," Alicia, age 30 said.
Butler and all of the women I spoke with for this story who had hormonal IUDs said variations of the same thing: it's kind of nice not having a period. According to Planned Parenthood, not getting your period or only having light bleeding while using an IUD is "totally normal and safe," however some women will still get a period.
There are at least four brands of hormonal IUDs available today including Mirena®, Liletta, Kyleena®, and Skyla®. Meredith, 33, said she's had two Mirenas and two Skylas. "Mirena made me feel robotic emotionally," she said.
While it hasn't been medically proven (and is denied by the brand), some report something called colloquially "the Mirena crash" which usually refers to feelings of depression after removing it. Meredith says that after switching to Skyla, her mood returned to normal.
One of the most robust studies on the link between depression and hormonal birth control (it surveyed over a million women living in Denmark) found that women on hormonal birth control were more likely than those who were not to be on antidepressants. About 2 percent of women on hormonal birth control methods—including IUDs—were prescribed antidepressants in a year, compared with 1.7 percent of women who were not using hormonal birth control.
However, that is not to say depression is the norm with hormonal IUDs; most people will experience very few side effects. Butler said a common side effect of hormonal IUDs is," intermittent spotting especially in the first six months after insertion," however she usually recommends the hormonal IUD for patients. "I generally lean towards hormonal IUDs because of their effects on menstrual bleeding. If there is heavy bleeding I will recommend hormonal to improve bleeding. If the patient wants a non-hormonal option then I'll use the copper IUD," she said.
Copper IUDs
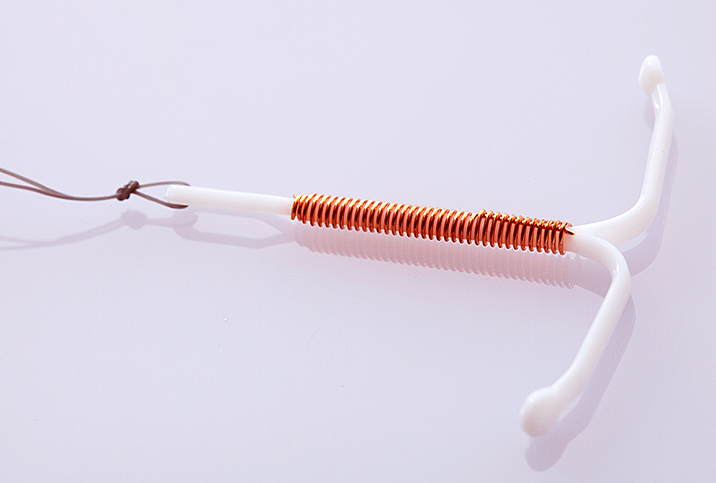
On the outside, a hormonal and copper IUD look basically the same; they are both T-shaped pieces of plastic (to me they look like if someone 3D printed a tiny picture of a uterus). The difference is that the trunk of the copper IUD (Paragard is the brand available in the USA) has copper wire woven around it; copper produces a reaction inside the uterus that kills sperm.
Heavy bleeding is a side effect of the copper IUD. Lily, 34, said, "My copper IUD made me bleed heavily. I had heavier periods and would bleed in between periods. My gynecologist recommended I switch to the non-copper. It was annoying to get one out and another in (I find the process painful) but I'm glad I did. Once I switched, the bleeding stopped."
Anecdotally, the two women I spoke to who had IUDs and had vaginal childbirths said they did not find insertion painful post-birth.
Unlike Lily, Joanna, 38, has had no side effects from her copper IUD, except slightly heavier periods (she says hers were light to begin with so this change is manageable). "I like not thinking about it, and not having my hormones manipulated," she said.
In rare cases, the Paragard has reportedly broken inside the body, resulting in sometimes serious conditions.
Is there anyone who shouldn't get an IUD?
Most people who are trying to prevent pregnancy can benefit from an IUD (and if the idea of an IUD freaks you out, Nexplanon is another long-acting birth control that's inserted into the arm; I used to have this and I loved it).
"The only people that I caution against IUDs are patients that don't practice safe sex. An STD can easily turn into PID [pelvic inflammatory disease] if an IUD is in place. I caution every patient that practicing safe sex is a must," Butler said.
If you're planning to try to conceive in the next year or two, getting a new IUD may not make sense from a financial standpoint. "It is not cost effective to place in a patient that only wants to use it for a year but some patients really like the convenience of it," she said.