How to Manage Living With Urinary Incontinence

Everyone's born incontinent. As babies, the processes of urination and defecation are completely outside of our conscious control. As we mature, the body develops various functions meant to ensure some level of autonomy when answering nature's call. As we age further, however, things might begin to go wrong again for various reasons.
In clinical practice, there are two types of incontinence: bowel incontinence and urinary incontinence (UI). Here, we will focus on bladder control problems, or urinary incontinence—how to live with and prevent it, and the impact it may have on life, relationships and general well-being. Plus, we'll debunk a few myths about UI.
What are the types of urinary incontinence?
Urinary incontinence is described as the involuntary leakage of urine. Anyone who seeks medical intervention for bladder control problems may be given a UI diagnosis.
The type of UI a person displays has a direct impact on their quality of life. In general, urinary incontinence can have a significant negative impact. Beyond the hygienic issues to worry about, there are sexual, psychological and social factors to consider.
Too many UI patients avoid seeking medical counsel due to shame or embarrassment. Urinary incontinence is fairly common, and healthcare providers deal with this condition frequently, so be direct and honest with your primary care physician if UI is causing undue distress in life.
There are five broad types of urinary incontinence, and each presents in unique ways:
- Stress incontinence. This type is typically caused by weak bladder and pelvic floor muscles. Patients with this type of UI may leak urine during certain activities, such as jumping, running, coughing, laughing or sneezing. It's mostly observed in women.
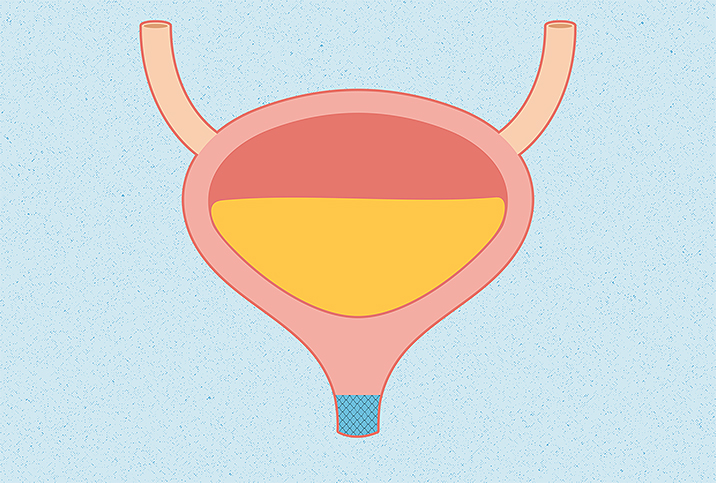
- Urge incontinence. Sometimes referred to as overactive bladder, urge incontinence is typically described as a strong or sudden urge to urinate that gives people very little time to react. It may be caused by the random contractions of an overactive detrusor muscle (the muscle that surrounds the bladder).
- Mixed incontinence. It is not uncommon for patients to exhibit symptoms of both stress incontinence and urge incontinence at the same time.
- Overflow incontinence. This type is the opposite of urge incontinence and is sometimes referred to as a lazy bladder. It may occur when the detrusor muscle that surrounds the bladder fails to contract or when there's a blockage of the urethra caused by an enlarged prostate (typically observed in older men).
- Functional incontinence. This type is typically observed in frail elderly patients. It's caused by underlying mobility issues or disabilities that make it difficult to get to a toilet in a reasonable time without assistance. Although urinary incontinence is very common in the elderly, keep in mind that it is not considered a "normal" part of aging.
"If you're experiencing any kind of bladder leaks, we recommend you speak with your doctor who can help identify the causes and establish the best treatment plan," said Jeannine Miranne, M.D., a urogynecologist at Brigham and Women's Hospital at Harvard Medical School in Boston.
Women are more likely to develop UI than men.
As with almost any condition, a diagnosis of incontinence can be difficult to accept, according to Aleece Fosnight, M.S.P.A.S., a board-certified physician's assistant and a medical advisor at Aeroflow Urology in North Carolina. And also as with other conditions, you need to understand why you might have a diagnosis of incontinence.
"Finding support groups in your area can be reassuring that you are not alone through this journey. If there isn't one in your area, consider starting one," Fosnight said. "There are podcasts and website resources that can help guide you to finding ways to support yourself. Talk to your loved ones and trusted friends. These conversations can be tough, but are needed to move through the emotions that come with a diagnosis of incontinence."
People can experience some frustrations after an incontinence diagnosis, Fosnight said.
"Talking to a mental healthcare provider—therapist, psychologist, counselor—can be helpful in working out your emotions and dealing with grief, loss and moving forward in a positive light to enhance the quality of your life," she said.
Many non-invasive strategies can help patients regain continence for both stress and urge incontinence. These include the following:
- Kegel and pelvic floor exercises
- Yoga
- Mindfulness-based stress reduction
- Prompted voiding
- Quitting certain bladder irritants such as caffeine and alcohol
- Smoking cessation
- A weight loss regimen
These strategies fall under the category of behavioral therapy and could also help reduce the frequency and severity of a patient's UI episodes. In fact, experts claim that behavioral therapy has been used in UI treatment since the 1940s and has been shown to reduce UI frequency by 57 percent to 86 percent.
If non-invasive strategies don't work, a healthcare professional may offer pharmaceutical or surgical alternatives, depending on the specific type of UI on display.
What happens if you don't address your UI?
In general, neglecting to seek counsel and failing to address your UI over long stretches of time could significantly worsen your well-being in many ways.
Diminished sexual desire and frequency
Women are more likely to develop UI than men. This is partly due to anatomical differences between the two genders, namely a shorter urethra in women.
While pregnant or postmenopausal women are most at risk of UI, even young, active women can experience it. Studies have shown that a significant number of elite female athletes report stress urinary incontinence. Sexually active women living with UI have been shown to report the fear of leaking urine during sex, leading to increased anxiety and loss of vaginal sensation, among other symptoms.
Men with partners who suffer from UI also reported less sexual satisfaction, which shows how UI can be damaging to a person's relationship and sexual well-being if they don't address it.
Sleep deprivation
Urinary incontinence can strike at night and cause consistent disruptions to a patient's sleeping schedule, resulting in adverse effects on their quality of life. The relationship between sleep deprivation and urge incontinence is well established, according to a 2017 study, and is further linked to increased daytime fatigue, depression, anxiety and poor psychosocial health in general.
Productivity losses and costs
Not only can urinary incontinence potentially cause an increase in fatigue due to sleep deprivation, it can increase the frequency of your toilet breaks and cause your boss to question your commitment to the workplace. Additionally, not everyone has a conveniently located bathroom at work.
The direct and indirect economic costs associated with urinary incontinence also place a large burden on society, and researchers have shown that seeking treatment is cost-effective over the long term.
Myths and misconceptions about urinary incontinence
As a condition with a stigma attached to it, UI is surrounded by misconceptions that need to be addressed.
Myth #1: It only happens to older people.
Though urinary incontinence occurs more often as people get older, Miranne said, there are many other groups for whom UI is an issue, including people experiencing the following:
- Pregnancy
- Childbirth
- Menopause
- Enlarged prostate
- Prostate cancer
- Obstruction/tumor anywhere along the urinary tract
- Neurological disorders
Multiple sclerosis, Parkinson's disease, stroke, brain tumor or spinal injuries can interfere with the nerve signals involved in bladder control, which can lead to urinary incontinence.
There are other factors that increase your risk of developing urinary incontinence, according to Miranne:
- Being overweight
- Smoking/tobacco use
- Family history of UI
- Diabetes
- High-impact sports
- Uncontrolled asthma or other lung problems
Myth #2: You can use period pads to manage bladder leaks.
"Period pads aren't designed to absorb and wick away moisture caused by urine, which is quite different from blood," Miranne said. "Given their difference in viscosity, urine flows much faster than menstrual blood.
Bladder leaks require five times the absorption to effectively wick them away, she added.
"If you're wearing a period pad every day to manage urine leakage, it's more likely that you'll experience skin irritation from poor absorption and excess wetness," Miranne said. "Doctors often see women who wear period pads or panty liners who think they've developed a yeast infection when really it's contact dermatitis or what we would call a 'diaper rash' in babies, caused by the products they are misusing to manage their leaks."
Myth #3: It's not treatable.
There are a variety of options for the treatment of urinary incontinence.
"Treatments vary in invasiveness and depend upon the type of incontinence you have," Miranne said. "This is why it is important to consult with your doctor, so that he or she can provide you with the right options for treatments for you."
Myth #4: If your body is muscular or strong, your pelvic floor must be strong.
"Pelvic floor dysfunction can occur in athletes and other otherwise physically fit women, even women who do a lot of core strengthening," Miranne said. "In fact, it's quite common for high-impact exercise to trigger bladder leakage."
The pelvic floor muscles do, however, respond to strength and endurance training like other muscles in the body, said Melissa Nassaney, D.P.T., P.T., a board-certified women's health clinical specialist in Warwick, Rhode Island.
"It is not something you have to 'just live with' because you had a baby," Nassaney said. "If you tried Kegels in the past and they 'didn't work,' most likely they were performed incorrectly or you need additional training in exercise other than Kegels, or in addition to kegels."
For example, someone with significant hip weakness due to pain and arthritis may have a good kegel squeeze on command but still leaks because of pain and weakness in the hip that requires more effort to walk, get out of a chair, car, etc. That can cause more strain on the bladder from the abdominals and low back to support movement or activity, impeding normal bladder control.
"Sometimes, a kegel is good on the spot with a kegel squeeze but less effective during a bout of a cough attack or laugh attack," Nassaney said.
UI can come and go
In many cases, urinary incontinence is dynamic, which means it alternates between periods when everything is fine (remission) and periods when the bladder starts acting up again. It could be bothersome but temporary and be triggered by menopause, prostate surgery or pregnancy, among other things.
However, it could also be chronic and seriously disruptive.
The severity and frequency matter, and if your urinary incontinence is chronic or the leaks are significantly voluminous—usually seen in urge incontinence—then it is best to consult a doctor.
"Undiagnosed incontinence usually causes more social and activity limitations along with withdrawal, depression and anxiety," Fosnigt said. "Wearing pads for incontinence is a prime environment for bacteria and can lead to urinary tract infections. Urine is also very irritating to the skin and can cause skin breakdown over time with prolonged exposure.
"If urinary retention is the cause, this can lead to urinary tract infections as well as reflux to the kidneys, causing kidney failure. If urinating is not possible, this could be an emergency, and catheterization is usually needed."
Although urinary incontinence is not life-threatening, it can be bothersome and affect your dating life, depending on the type of UI and its frequency and severity. A proactive approach, with the help of a healthcare professional, can identify the best strategy to prevent and alleviate symptoms in order to restore continence and make you more confident to put yourself out there in the dating world.
"Education is a huge key to prevention," Fosnight said. "Most of my patients report being told, by healthcare providers mostly, that their incontinence symptoms are normal. Or, unfortunately, patients do not bring up their concern with incontinence, again because of embarrassment.
The key to thinking about prevention is to know the risk factors. Those risk factors, according to Fosnight, include
- Pelvic floor dysfunction
- Constipation
- History of pregnancy
- History of pelvic surgery (e.g., hysterectomy, prostate, GI)
- Peri/menopause status
"Just because something is common does not mean that it is normal. No one should have to live with incontinence," she said. "Prevention options include seeing a pelvic floor physical therapist, avoiding constipation, staying hydrated with water, avoiding bladder triggers, not straining to empty the bladder and trying not to void more than every two hours, if you can."
That said, don't necessarily avoid the urge to void, either, especially if it has been longer than two hours.
"Talk to your healthcare provider about your concerns with developing incontinence if you have any of the risk factors," Fosnight said. "Most of the time, a referral is not needed to see a pelvic floor PT."
Other resources for help with UI
Given the number of people who develop urinary incontinence, nobody needs to suffer alone or in silence. Look for information and help at the following organizations:
- American Urological Association (AUA)
- Urology Care Foundation
- The National Association for Continence
- The National Institute on Aging
- Bladder & Bowel Community
- The International Continence Society podcast
- The American Urogynecologic Society (specializes in female urinary incontinence)
- Pelvic Floor Guru