The Frequency of Diagnosis and Risk Factors of Urinary Incontinence

When doctors speak of incontinence, they're usually referring to one of two conditions: bowel incontinence or urinary incontinence (UI). Both are caused by the body's inability to contain its waste products.
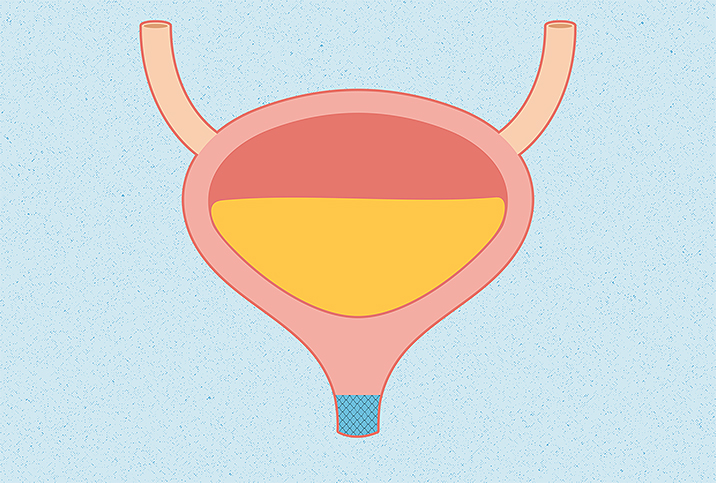
Here, we will focus on bladder control problems—urinary incontinence—the underlying factors that lead to it, the populations most often affected and the impact it may have on sexual health.
What is urinary incontinence and what are the types?
The definition of UI is fairly straightforward. Urinary incontinence is described as the complaint of any involuntary leakage of urine. If you've ever accidentally leaked urine and it caused you to seek medical intervention, it qualifies as urinary incontinence.
A doctor will then need to further identify the type of UI a patient exhibits. There are five broad categories:
- Urge incontinence (aka overactive bladder) is characterized by a very strong urge to urinate followed quickly by an involuntary draining of the urine contained in the bladder.
- Stress incontinence is characterized by small to moderate leaks caused by triggers such as sneezing, laughing, coughing or physical exercise. It's generally observed in pregnant women and athletes.
- Mixed incontinence is a mixture of urge and stress incontinence characteristics.
- Overflow incontinence is characterized by a blockage or weak bladder muscles that cause a constant dribble or leak of urine. It's commonly observed in older men with prostate issues.
- Functional incontinence is not caused by bladder issues but by mobility problems (such as arthritis) that may prevent the patient from getting to the toilet within a reasonable amount of time.
To treat or manage UI, doctors need to know the type. Healthcare providers also need to assess the severity and frequency of the leaks.
"Different triggers are linked to different types of urinary incontinence. The cause and type of incontinence one experiences will also affect the treatment that is recommended or most effective for each person," said Jeannine Miranne, M.D., a urogynecologist at Brigham and Women's Hospital at Harvard Medical School in Boston.
Persistent urinary incontinence can be caused by aging, obstruction, obesity, smoking and neurological disorders for both sexes, according to Miranne.
"Temporary urinary incontinence can be caused by certain foods and drinks (alcohol, caffeine, carbonated drinks, spicy foods, acidic foods, sweeteners)," she said. "Other factors that can lead to temporary urinary incontinence include UTIs and constipation."
A person's bladder and urethral sphincter muscles may naturally weaken over time, leading to the inability to properly control urination, Miranne added. When it comes to obstruction, tumors or urinary stones can block the normal emptying of the bladder and thus lead to overflow incontinence.
Obesity can put added pressure on the bladder and/or urethra. Smoking—tobacco is a bladder irritant—and neurological disorders such as multiple sclerosis can cause problems with the nervous system, including the nerves in charge of bladder function and control.
Risk factors of urinary incontinence
Urinary incontinence is usually a dynamic condition, not static. Its incidence rates are high, but so are remission rates. Patients with UI tend to alternate between continence and incontinence rather than continuous chronic incontinence.
This is further highlighted by the fact that global prevalence among older women is between 3 percent and 53 percent. Such a wide range of data hints at the dynamic nature of UI.
"While incontinence can affect anyone, women are more than twice as likely to experience UI when compared to men," Miranne said. "When examining the causes of incontinence in women, we think of things that are a natural part of the biologically female experience."
Women's pelvic floors are more vulnerable to injury as a result of several factors—pregnancy, childbirth, menopause, hysterectomy—that increase the likelihood of developing UI, Miranne said. Changes in hormones and a growing child's weight can put pressure on the pelvic floor, leading to urinary incontinence. When it comes to surgery, the removal of the uterus (hysterectomy) can affect pelvic nerves involved with bladder control.
Women's estrogen production decreases after menopause, and declining levels can contribute to incontinence. Vaginal birth can contribute, too, as it can weaken the pelvic floor muscles and may even damage the pelvic nerves and lead to pelvic organ prolapse, which commonly co-occurs with incontinence.
Ethnicity as a risk factor for incontinence
A person's ethnicity seems to play a role as well. Some researchers suggest that anatomical and physiological differences between groups may help explain the difference in prevalence rates around the world. For example, a study in Malaysia found Chinese women to be 60 percent less likely to experience UI compared to the majority Malay population.
Studies in the United States have also shown non-Hispanic white women to be the most at risk of urinary incontinence. However, more research is needed to help explain these differences.
UI can be caused by a variety of factors. It isn't a life-threatening condition, but it can cause social, psychological and hygienic issues that may significantly diminish a person's quality of life.
The condition is significantly more common in women according to researchers, and this is especially true as they age. Prevalence data in the U.S. places UI somewhere between 30.8 percent and 36 percent for older women, while some studies put the number as high as 60 percent.
Other studies have claimed that UI occurs in roughly 40 percent of women over the age of 70.
Rates are much lower in older men at an estimated 6 percent, roughly five times less than older women. When men age, they are more likely to develop prostate problems, which may lead to blockages, urinary tract symptoms and other related conditions, according to experts.
Older people are not the only demographic at risk of urinary incontinence, though. Researchers studying elite young athletes have suggested that nearly 33 percent of them experience UI, with female athletes being 5.45 times more likely to present UI symptoms compared to their male counterparts.
A majority of the cases were described as stress incontinence, mainly caused by jumping, running or "different situations."
Since stress incontinence may affect active young women, researchers have tried to study the impact this may have on their sexual function. The data is not encouraging and largely shows impaired sexual functioning, which may cause many women to avoid sex altogether.
It is believed that nearly 50 percent of sexually active women with UI experience some form of female sexual dysfunction, and may report the following:
- Problems with orgasm and vaginal lubrication
- Reduction in sexual desire, excitation and satisfaction
- Greater sexual avoidance
- Diminished mental well-being
- Body image insecurities
- Reduced motivation
- Anxiety over smelling like urine
- Fear of urine leakage during sex (which causes tension)
- Loss of vaginal sensation
Studies involving couples have shown that men who have a partner with UI report less sexual satisfaction in their relationship compared to men who have a partner without the condition. These findings make sense when you consider the fact that many women with UI report a diminished sexual drive/desire, leading to a reduced frequency of sex, and therefore a potentially unsatisfied partner.
"Some women do leak during sex and so do men after prostatectomy; it happens," said Melissa Nassaney, D.P.T., P.T., a board-certified women's health clinical specialist in Warwick, Rhode Island. "Leakage can be very unpredictable. In some situations, you just need to plan for it and/or talk about it with your partner."
Unfortunately, some people may avoid all intimacy due to embarrassment, according to Nassaney. Some ignore intimacy and focus on other aspects of a relationship.
"Although understandable and a matter of choice for some, there are others who do not want to put aside their sexual health but feel really inadequate to address the barriers and not sure how to bring it up to their doctor or partner," she added.
Talk to a professional about UI
Anyone suffering from urinary incontinence should be blunt with their doctor. UI is common and there is no reason to feel embarrassed about speaking to a healthcare professional, especially when symptoms cause significant distress to your everyday life.
UI is not life-threatening and can be managed with a proactive approach. Keep in mind, though, that treatment options may vary depending on the severity and type of UI a patient displays. You shouldn't feel ashamed to open up to a professional if urinary incontinence is negatively affecting your quality of life or sexual health.
"For incontinence issues, I usually recommend someone that has a urology background—urologist, urogynecologist, or other healthcare providers (P.A.-C.) in a urology specialty," said Aleece Fosnight, M.S.P.A.S., a board-certified physician's assistant and a medical advisor at Aeroflow Urology in North Carolina. "Some gynecologists have more incontinence knowledge and would encourage you to start the conversation with your provider.
So when should you seek help?
"Before there is a problem," Fosnight said. "[Especially] if you have risk factors including pelvic floor dysfunction, constipation, history of pregnancy, history of pelvic surgery (hysterectomy, prostate, GI, etc) and peri/menopause status. Prevention is the key to incontinence.
"Remember, just because something is common does not mean that it is normal. No one should have to live with incontinence."