The Impressive Evolution of IVF and Fertility Treatments
It's hard to believe that the first baby conceived and born in the United States with the help of in vitro fertilization (IVF) turned 40 on Dec. 28, 2021.
What was considered at the time a novel and unusual procedure has become a widely accepted—and constantly improving—pregnancy method for couples or individuals who are unable to conceive without the help of medical intervention.
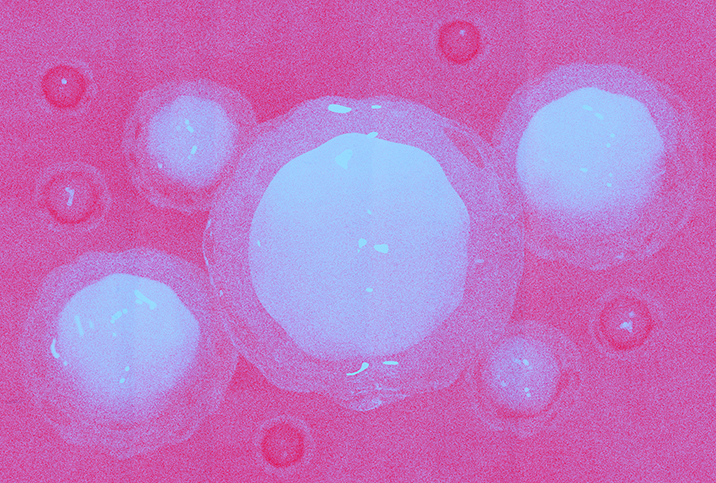
One in 8 couples face infertility, according to the Centers for Disease Control and Prevention (CDC), and hundreds of thousands of these couples undergo IVF each year in the hope of becoming pregnant. During IVF treatment, mature eggs are retrieved from the ovaries and sent to a lab to be fertilized by sperm. After fertilization, the eggs become embryos and are implanted into the uterus where one or more may develop into a fetus. Couples may need several rounds of IVF for a successful pregnancy.
Aside from IVF's novelty fading away with the passage of time, much has changed between Elizabeth Carr's birth in 1981 and the reality of IVF and other fertility treatments in 2022. However, with technology advancing and the healthcare system continuously in flux, there's a long way to go and even more ways to improve the availability of fertility treatments for people looking for assistance.
Here's what you need to know about IVF then, now and in the years to come.
The science of fertility is only about 100 years old
"The interesting thing about IVF is that we really started with what a hormone was. We didn't understand what estrogen or progesterone was until about 1920. We didn't understand that there were hormones that the body responds to," said Jane L. Frederick, M.D., a board-certified reproductive endocrinologist at HRC Fertility in Orange County, California. "Then in the 1950s and 1960s, we were able to start growing embryos in an animal model, in a rabbit model, but it's tough to translate the rabbit model to humans. We had to learn how to grow an egg, how to extract it. An egg needs different nutrients at different stages in development."
This is all to say that fertility is complicated; much more complicated than most people imagine, especially when the often credited "birds and bees" make it appear simple. Sure, "sperm meets egg" is a critical part of the process, but recreating the process of conception outside the human body isn't something that just happens with the clapping of your hands.
In fact, it wasn't until the late 1970s that scientists in the United Kingdom were able to successfully transfer an embryo into a human uterus. This resulted in the first-ever IVF baby—called a "test-tube baby" back then—Louise Brown, who was conceived and born a few years before the science was successfully reproduced, so to speak, in the United States with Elizabeth Carr.
"It was a breakthrough at the time because we didn't understand that women were suffering from infertility. Brown's mom had blocked tubes. The birth of Louise Brown allowed us to be sensitive to women who are having fertility issues," Frederick said.
It's this understanding and empathy that have helped open up a world of treatments for people dealing with infertility in the 40 years since IVF was first implemented in the United States.
A better understanding of fertility, and more treatment options
When scientists started recognizing the fertility challenges that many men and women face, it opened up doors to more expansive research.
Where IVF treatments started as a way to offer a chance of reproduction to a woman with blocked fallopian tubes, now medical fertility specialists help identify, address and treat a broad range of underlying issues that may lead to infertility. These specialists are typically medical doctors who have undergone a four-year OB-GYN residency followed by a three-year reproductive endocrinology fellowship.
According to Frederick, doctors can treat so much more than tubal complications now.
"We can treat endometriosis or low sperm count. We can help women with recurring miscarriages who can get pregnant but can't have a full-term pregnancy," Frederick said. "We treat a lot of patients who are over 40….We can freeze an egg or freeze an embryo. That process has helped single women who don't have a partner be able to maintain their biological options for the future. We can treat cancer survivors; we can preserve their fertility.
"The science went from 'this person has blocked tubes' to now treating gay and lesbian partners to provide options for fertility," she added.
How the science has changed and how the knowledge of female fertility has grown is truly amazing.
"I've been in practice for the last 30 years," Frederick said. "The historical perspective on how much has changed is critical. It's about reproductive choices. We're good about birth control: 'Prevent a baby, take this pill.' We don't talk a lot about reproductive choice, about deciding to freeze the biological clock at this time."
IVF and other fertility treatments offer choices
Really, the field of fertility is about offering choices. Offering choices to single women who want to have children. Offering choices to same-sex couples. Offering choices to couples struggling to conceive. Offering choices to people who want to have children "not now, later," without knowing when later will be.
But what's also important to recognize is that IVF is almost never the first option. Depending on the underlying cause of the fertility challenge, the solution could be quite simple and relatively inexpensive.
"Forty percent of the time, [female] infertility is an ovulation problem. The woman's not ovulating. This can be treated with Clomid [an estrogen modulator] to help with ovulation," Frederick explained. "Forty percent of the time, it's that a man's sperm count is too low or not moving well—it's a male factor issue. We can treat that by finding out why, and we can do artificial insemination to allow the best sperm to meet the egg at the right time."
For about 15 percent of couples, testing shows that everything is normal. This is called unexplained infertility. These patients have a high chance of success without treatment, with up to 80 percent conceiving within three years, according to research compiled by the Royal College of Obstetricians & Gynaecologists in London.
Other individuals who seek help with fertility challenges include women who get pregnant but miscarry, and patients older than 40 who ovulate but whose eggs aren't good due to age, Frederick said.
"There may also be genetic-related conditions we can prevent through technology, or same-sex couples who can't conceive biologically without assistance," Frederick added.
The point being, many of these patients can be treated without more intense medical interventions, such as IVF.
Success rates have improved significantly
Success rates for fertility treatments are constantly improving. The science and understanding are better, and doctors are able to reduce challenges that were common early in the procedure's inception.
"When I first started practicing, we didn't have a lot of knowledge about how to grow an embryo and we were putting embryos back into the mother at day two or day three of development," Frederick said. "We were putting back more embryos to try to increase the likelihood of success, but we were getting a lot of twins, triplets and quads, which are often born as preemies and who don't do well in the NICU and can end up with lifelong disabilities."
As the science has expanded, doctors have been able to start transferring embryos back into mom at day five, by which time many unhealthy embryos have "self-selected" out, leaving the healthier ones for transfer. This process has resulted in fewer risky multiple births and more healthy, full-term pregnancies.
Genetic testing is impressive and still in its infancy
Another way that fertility treatments, and specifically IVF, can provide choices to parents is through genetic testing. This field of study is a bit controversial in that naysayers claim it's a way to conceive "designer" babies through the selection of specific traits, including sex, hair or eye color. But really, for people who have a known genetic predisposition to medical problems, genetic testing can be a way to ensure the baby won't be predisposed to those problems.
"I think the genetic testing in itself will allow the success rate of IVF to go way beyond where we are now," Frederick said. "We are getting better and better at identifying issues related to genes and the knowledge of gene characteristics. For instance, sickle cell disease. We've been able to figure out which gene it's on, and there's a procedure called CRISPR which allows genetic engineering to cut out the damaged sickle cell gene and replace it with a healthy gene. It would be phenomenal if we could eradicate sickle cell disease."
The CRISPR process is in experimental stages, according to Frederick, but she noted that continuing research into embryo genetics will allow fertility specialists to better select embryos in the future.
"Probably not for the next 20 years, but maybe our children might have the opportunity," she said.
The ongoing issues of cost and insurance
Unfortunately, the cost of IVF treatments remains high, and the insurance coverage available to patients tends to be scarce or inconsistent.
"Only 30 percent of my patients have coverage for fertility through their insurance plan," Frederick said.
She sees this as an area where lobbyists, doctors, companies and individuals need to push for more assistance.
"As women, we need the freedom to decide when we want to preserve our fertility. [Infertility] is a disease, and everybody should have the right to treatment. There should be universal protection for fertility," she added.
Frederick is not the only one to address the financial challenges associated with infertility and its possible treatment options.
"Availability is still an issue because from country to country and state to state, the insurance coverage is not the same. This makes it difficult to level the playing field," said Elizabeth King, a certified fertility health coach, birth and bereavement doula and new parent educator in California. "In some cases, people have access to up to six rounds of IVF through their insurance policies. Others have to pay out of pocket."
With the cost of a single round of IVF averaging more than $12,000, this option is out of reach for many couples. But King said awareness and the advent of social media have helped make paying for IVF more feasible, even for people without insurance coverage.
"Many companies now offer grants and loans for IVF and surrogacy," King said. "Interest has also changed in recent years, partially because of the internet and social media. I have seen people do GoFundMe pages and get loans and grants and successfully get the family they have dreamed of."
Ultimately, however, relying on grants or loans isn't helpful to all individuals facing fertility challenges. Fighting for health care that universally covers the cost of treatments remains a high priority for professionals in the field who believe all people should have a chance at building a family of their own.
Maintaining hope through the struggle
One issue that both Frederick and King emphasized is the importance of mental health for infertility patients. Despite increased awareness of infertility, stigma remains around the issue, and a lack of hope can negatively impact a person's success with fertility treatment or even their willingness to seek treatment.
"Mental health is a huge barrier in fertility," King said. "It's not talked about, and that's a big disservice to patients. Studies show that women have increased results with the help of someone like a coach or therapist during their journey."
The psychological symptoms associated with infertility are the same as those of a cancer patient, according to a 1993 study in the Journal of Psychosomatic Obstetrics and Gynaecology authored by Alice Domar, Ph.D., a leader in the field of mind/body medicine and infertility, and professor at Harvard Medical School in Boston.
Frederick agreed that hope is incredibly important to emphasize to patients who are struggling to conceive.
"I hear it a lot from my patients: they're depressed, frustrated; they get a lot of negative feedback from their families. They see all the Mother's Day and Father's Day hype. There are a lot of external factors that cause depression in my couples," Frederick said. "But it's important that they don't give up hope. As long as they're open to coming in and being evaluated, there really is hope for many of the patients."
In reality, if they're financially able to seek testing, most couples end up being successful with fertility treatments.
"Testing can be done right away within the woman's next cycle, the next four weeks. Tests can tell me if there are eggs available and what quality they are. There's an X-ray that tells me if the tubes are open. We can order a sperm test analysis," Frederick said.
In other words, if you're able to access help, the right approach and treatment are often available.
It's also important to be aware of the reality of the biological clock. If you're younger than 35 years old, seek a doctor's help after a year of trying to conceive without success. If you're between 35 and 40, give it only six months. If you're older than 40 and attempting to conceive for the first time, Frederick said it's best to seek tests immediately to make sure you know what you're dealing with. As far as fertility advancements have come, biology remains a reality, and it's still more difficult to become pregnant with advancing age.
At the end of the day, it's helpful to know what fertility treatments are available and to understand the options you have based on your insurance plans and financial situation. If you're concerned about your fertility, don't hesitate to consult your OB-GYN or a fertility specialist to undergo tests that can help ease your anxiety and provide a course of action for long-term family planning.