IUD-Related Pain Needs to Be Taken Seriously

When Ivy Lovejoy, 22, from Utah, decided to get a hormonal intrauterine device (IUD) to control period pain and symptoms of polycystic ovary syndrome (PCOS), she didn't expect the pain of its insertion to be so intense that she would almost pass out.
"When they started opening my cervix, it was a stabbing pain because they had to keep trying different sizes, which led to burning from so much stretching," Lovejoy said. "As they inserted it, it started throbbing, and I nearly blacked out from the pain."
Even after enduring the pain of insertion, her body rejected the IUD within three months. Her body's attempt to push it out resulted in the device getting stuck in the top opening of her uterus, which resulted in a large cyst forming on her left ovary and numerous bladder infections.
"Now my bladder is permanently damaged to a point that I can barely hold my pee, and I have to constantly pee about every 15 to 30 minutes," she said.
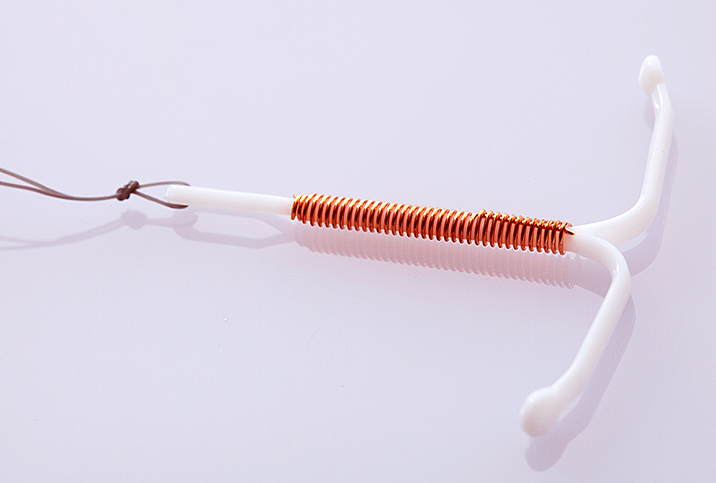
IUDs are more than 99 percent effective in preventing pregnancy for up to 12 years, depending on the kind of IUD. This small margin of error makes the IUD a popular choice, with an estimated 14 percent of women between the ages of 15 and 44 using one.
However, while the pain of inserting an IUD is unremarkable for some people, it can be excruciating for others. A 2013 study published in Human Reproduction Update stated that 17 percent of women who had not previously given birth, and 11 percent of women who had, experienced substantial pain during insertion that needs to be proactively managed.
Traci Kurtzer, an OB-GYN with Northwestern Medicine in Chicago, explained that the level of pain after insertion can vary from one patient to another, but the majority likely feel some cervical pinching or intense uterine cramping. Some patients have severe uterine pain and may even have a vasovagal response to the procedure, leading them to pass out.
A sign that the IUD may be displaced or at risk for expulsion is severe cramping, especially if accompanied by heavy bleeding, that is not responding to over-the-counter nonsteroidal medications.
"In my practice, I inform all my patients that I can't predict how much pain they may have, so if they choose to do placement without sedation, we should have them best prepared to handle any discomfort with medications to reduce cervical pain [and] uterine cramping and lessen anxiety," she said.
A lack of pain management options
Some practitioners recommend taking ibuprofen before the procedure, but some research indicates this approach does not actually reduce pain during IUD insertions. In fact, a 2009 study published in the Cochrane Database of Systematic Reviews reported that both nonsteroidal anti-inflammatory drugs (NSAIDs) and misoprostol did not reduce pain during IUD insertion. The study concluded no interventions that had been properly evaluated to that point reduced pain during or after IUD insertion.
Anxiety regarding the procedure and the painful experiences of peers during IUD insertions can also put people on edge. According to Kurtzer, talking patients through the procedure and creating opportunities for them to stop in between steps can help instill trust in the practitioner and manage pain better.
"I remind them we can stop the placement at any point up to when the IUD is already in the uterus. I gauge how they are doing with pain control in the steps prior to actual placement and recheck to make sure they want to proceed with each next step. If they are really not coping well with the pain, I stop the procedure and we discuss the options," she explained.
Kurtzer specializes in treating patients who have experienced sexual and medical trauma, and all of her patients are offered IUD placement under sedation if they prefer.
For some people, the pain is ongoing
In cases where the body rejects the IUD, pain may persist after the initial insertion. A sign that the IUD may be displaced or at risk for expulsion is severe cramping, especially if accompanied by heavy bleeding, that is not responding to over-the-counter nonsteroidal medications. Another sign might be feeling the tip of the IUD in your cervix or the strings lengthening, according to Kurtzer.
However, in many cases, including Lovejoy's, these symptoms aren't enough to convince a doctor to remove the device.
"He 'didn't want to waste a good device' despite the pain I was in and the constant infections," Lovejoy said, adding she was not taken seriously until she saw a different doctor, who took out the IUD as soon as she saw how bad the infection was. However, the damage was done, and Lovejoy now deals with severe urinary continence.
Jessika Ralph, a complex family planning specialist and OB-GYN in Minnesota said it's hard to generalize why a physician may choose to not take out an IUD.
"I would hope it is because the healthcare practitioner knows, based on the studies available, that with time, around six to 12 weeks, most patients find the side effects of the IUD tolerable and are finally experiencing its benefits: minimal bleeding or no periods at all, minimal or no cramping," Ralph said.
However, she said practitioners need to remember that each patient's experience is unique, and if they request an IUD removal, it should be taken out, regardless of the reason.
"A lot of people don't realize that it is painful and very traumatic for a lot of us with vaginas," Lovejoy noted. "But it is also a last resort for a lot of us, as well, since other methods don't work for treating menstrual/PCOS/endometriosis symptoms."
She added that she wants the entire conversation around IUDs to shift toward recognizing the pain they can cause after insertion and, subsequently, developing effective pain management programs.
For her part as a practitioner, Ralph said patients would indeed feel more empowered to discuss pain management with their provider if they knew more about the insertion process, and research will continue until more solutions are found.
"I hope that as we as a general public continue conversations about the health care of people that can become pregnant [and] people with uteruses, and our general knowledge of topics like periods, pelvic pain and sex improves," Ralph added. "This will help us all understand the myriad reasons why a person might choose an IUD or other form of contraception, as they all have many uses and benefits."