What Is Urinary Incontinence in Women?

The federal Office on Women's Health states that urinary incontinence affects twice as many women as men. This disparity occurs because the muscles that support the bladder and urethra in women may be affected by pregnancy, childbirth and menopause.
The National Association for Continence reports that urinary incontinence affects nearly 18 million women in the United States, but many suffer in silence. It can occur at any age but is more common in women older than the age of 50.
Urinary incontinence is a very common problem, and there is no need to manage it without help or be embarrassed about discussing it with your healthcare provider. The first step in managing incontinence problems is to reach out to your doctor for support.
Knowing that urinary incontinence isn't always a long-term problem is important. It could be temporary, caused by an underlying medical condition, or treatment may be available to fix the root cause. So let's look at the different types of incontinence and available treatments.
Types of urinary incontinence in women
Stress incontinence
"Stress urinary incontinence is the most common type of urinary incontinence in women," said Kecia Gaither, M.D., who is board-certified in OB-GYN and maternal-fetal medicine, and the director of perinatal services/maternal-fetal medicine at NYC Health + Hospitals/Lincoln in the Bronx, New York.
Although it's called stress incontinence, it's not related to mental stress. Urine leaks from your bladder when it's under sudden extra pressure, for example, when you cough, jump or sneeze.
Stress incontinence happens when the muscles that help prevent urination (such as the pelvic floor muscles and the urethral sphincter) are damaged or become weak. The main symptom is leaking urine when you do an everyday activity such as heavy lifting, exercising, sneezing or coughing. This leakage could be anything from a small dribble to a large stream with no warning.
Urge incontinence
You may hear urge incontinence called overactive bladder.
"Urge incontinence is the second-most common type of incontinence, characterized by the unexpected loss of urine while suddenly feeling the urge to urinate," Gaither explained.
In other words, you often can't hold off going to the toilet and might have only a few seconds between feeling the need to pass urine and then passing urine.
Many occurrences, such as hearing running water, having sex, orgasming or having a drink, can trigger urge incontinence. Although you may be able to get to the bathroom in time, the urge can happen more than eight times a day in some women. It can also cause you to wake up at night to pass urine (nocturia).
Mixed urinary incontinence
"Mixed urinary incontinence is a term employing both types of symptoms from stress and urge incontinence," Gaither said.
You might get the symptoms of urgency and frequency but also leak urine when coughing or sneezing.
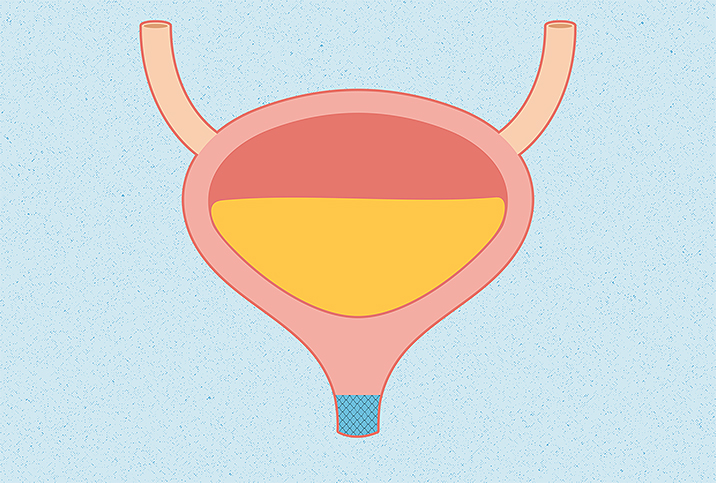
Overflow incontinence
Overflow incontinence is also known as chronic urinary retention. It usually means you pass tiny amounts of urine very often, and you may also feel as though your bladder is never fully empty.
With overflow incontinence, your bladder can't completely empty of urine, leading to bladder swelling. This happens because the bladder muscles are not able to squeeze properly to empty the bladder. Sometimes this is due to nerve or muscle damage from an injury, surgery or conditions such as multiple sclerosis (MS) or Parkinson's disease.
Functional incontinence
Functional incontinence happens as a knock-on effect of another condition, for example, if you have problems with your mobility due to rheumatoid arthritis. The problem isn't with your bladder or its surrounding organs, but you may not be able to reach the bathroom in time because of impaired mobility or confusion.
Total incontinence
When urinary incontinence is very severe and you constantly pass large amounts of urine, it is sometimes described as total incontinence.
What causes urinary incontinence?
We've touched upon the fact that urinary incontinence is more common in women due to events, such as pregnancy, childbirth and menopause, that put pressure on the pelvic muscles. But these are not the only causes.
Common causes include:
- Pregnancy (especially having multiple pregnancies)
- Vaginal births
- Requiring an episiotomy during childbirth
- Being overweight or obese
- Menopause
- Suffering from regular constipation
- Pelvic organ prolapse
- Damage to the bladder in surgery, for example, during a hysterectomy
- Neurological conditions, such as Parkinson's disease or multiple sclerosis
- Some connective tissue disorders, such as Ehlers-Danlos syndrome
- Certain medications
- Urinary tract infection (UTI)
- Too much caffeine
- A long-term cough
Getting older can also be a risk factor for urinary incontinence, and it's very common in women older than 80.
Diagnosis
When diagnosing urinary incontinence, Gaither said it's necessary to have an urogynecology evaluation and be assessed for a urinary tract infection, diabetes and neurological diseases to identify the problem and rule out any other causes.
Take note of your symptoms before you visit your healthcare provider, as they will ask you questions about:
- How often you go to the toilet in the daytime and nighttime
- If you pass urine when you cough, laugh or exercise or do similar actions
- How much you drink and the types of fluid you drink
- If you have any pain when passing urine, and if the urine is dark or smelly
- If you feel you can empty your bladder or it regularly feels full
- How much urine you pass when you go to the toilet; a lot or a dribble.
They will also ask about your medical history, family history and any medication you are taking. Sometimes you may be asked to keep a bladder diary if you are not sure about the symptoms you are experiencing and how often.
Depending on the cause of urinary incontinence and whether or not you respond to treatment, you may also need some further investigations, such as urodynamic tests or a cystoscopy.
Treatment
Treatment will depend on the type of urinary incontinence you are experiencing and the severity of the symptoms.
Gaither noted four main categories of treatment:
Behavioral
- Bladder training
- Scheduled toileting plans
- Diet modifications, such as reducing caffeine and bladder irritants
- Weight loss
Mechanical
- Pelvic muscle training, including treatment options like Kegel exercises, biofeedback, vaginal weight training/cones and pelvic floor electrical stimulation
- A vaginal pessary can be inserted into the vagina. It pushes against the vaginal wall and urethra to support the pelvic floor muscles.
Surgical
- Sling surgery is the placement of a sling around the bladder neck to help prevent leaking.
- Bladder suspension (colposuspension) involves lifting the bladder neck and stitching it in its lifted position to hold it in place.
- Nerve stimulation sends electrical signals to the nerves that control the bladder.
- An artificial urinary sphincter may be put in place if previous types of urinary incontinence surgery have failed.
- Urethral bulking agent injections are administered into the walls of the urethra to help it stay closed and prevent leaking.
- An augmentation cystoplasty is a surgery to make the bladder bigger to help treat urge incontinence, but you may need to use a catheter after this surgery.
Pharmacological
- Anticholinergic medications, also known as antimuscarinics, help stop the muscles in your bladder from tightening when they shouldn't.
- Botulinum toxin A, also known as Botox, can be injected into the wall of your bladder to help prevent overactivity in the bladder muscles.
- Vaginal estrogen helps strengthen the muscles and tissues supporting the bladder.
There is no need to suffer and live with urinary incontinence symptoms. With such a range of treatments for different types of urinary incontinence, the most important step is to speak to your healthcare provider. They can do a thorough assessment to find out your type of urinary incontinence and help you find a treatment plan that fits your lifestyle.
Practical tips to help with incontinence
If you are starting to notice signs of urinary incontinence, here are some tips to help stop leaking:
- Do daily pelvic floor exercises. Your healthcare provider, a women's health specialist or a physical therapist can teach you how to do pelvic floor exercises effectively.
- Learn how to lift. Tighten your pelvic floor muscles when doing any type of lifting. Avoid very heavy lifting when possible.
- Change your exercise regimen. Swap exercises that put pressure on your pelvic floor muscles, like running or high-impact aerobics, for strengthening exercises like Pilates or yoga.
- Stop smoking. Smoking can lead to coughing, which puts strain on your pelvic muscles.
- Eat a fiber-packed diet to help avoid constipation.
- Cut down on bladder irritants, such as caffeine, alcohol, citrus fruits and spicy foods.
- Drink plenty of water. Aim for at least six to eight glasses a day. An insufficient amount of water can cause the bladder to shrink, lead to bladder problems and worsen constipation.
- Maintain a healthy weight. Being overweight can weaken your pelvic floor muscles.