We Have Questions: Epididymitis
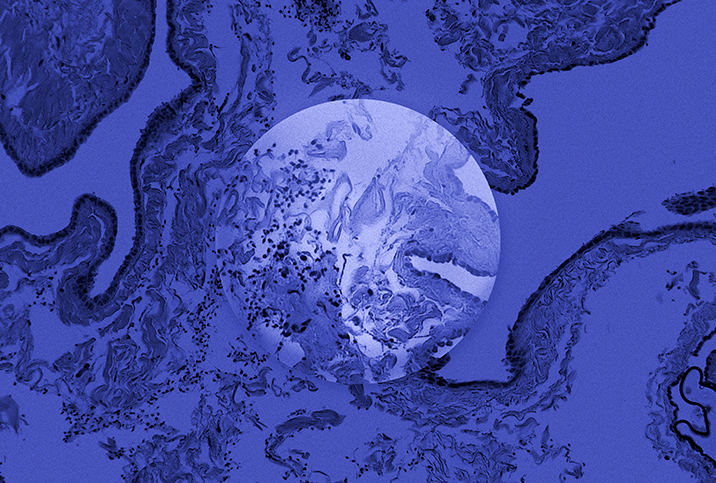
Testicles are more than simply a couple of egg-shaped structures that manufacture sperm and testosterone. They contain tubules, ducts, lobules, fibrous connective tissue and more.
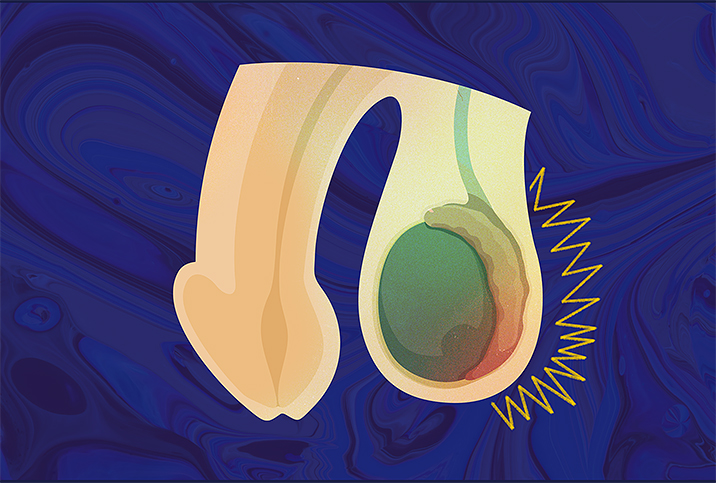
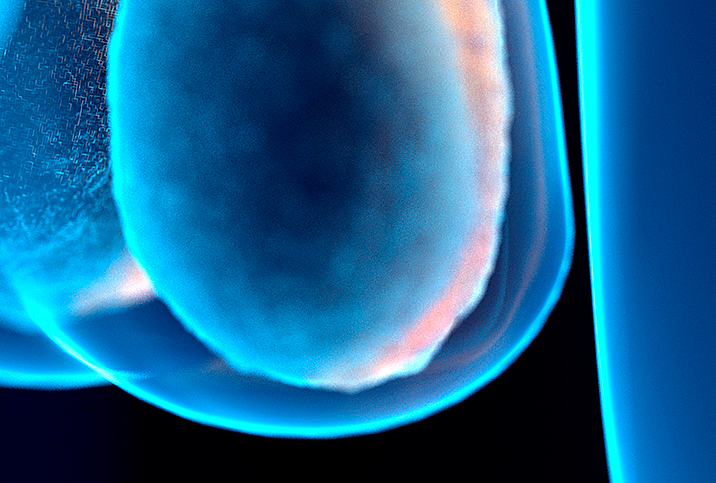
Attached to the rear of each one is an epididymis, a C-shaped duct that provides a safe space for sperm to fully mature after leaving the scrotal sac, but long before they are expelled during ejaculation or reabsorbed by the body.
Consisting of three parts—the head, body and tail—the epididymis is sort of a big spoon connected by efferent ductules, or minute tubes binding the testis to a network of ducts, channels and cords needed for ejaculation.
The epididymis head receives immature spermatozoa from the testicles and clings to the upper tip of the testes. Below, the tail tapers off to lead to the vas deferens, or the deferent duct, and eventually propels potent sperm in anticipation of ejaculation. Both ends of the epididymis resemble the tips of a crescent moon, while the body of the epididymis is the bulk of the crescent shape.
That middle part is specifically where immature spermatozoa incubate, a process that requires up to 14 days to complete.
Epididymitis is the inflammation and subsequent swelling of the epididymis, a condition experienced by more than 600,000 men of all ages annually, most commonly those between the ages of 14 and 35.
To find out more about this widespread condition of a relatively obscure bit of male genitalia, we spoke with Betsy Greenleaf, D.O., of Howell Township, New Jersey. Greenleaf specializes in the pelvic floor health of all genders, especially treating urinary pain or malfunction in the absence of a urinary tract infection.
What causes epididymitis?
Greenleaf: Most frequently, the inflammation is caused by bacterial infection but can also be caused by viruses, medications or irritant exposure, such as backflowing urine or irritation from increased activity that causes excessive scrotum movement. The most common bacterial cause in adults is sexually transmitted chlamydia or gonorrhea.
What risk factors increase the likelihood of developing epididymitis?
Medical conditions such as diabetes, being an older man, especially with an enlarged prostate, previous infections and engaging in penetrative anal intercourse can increase the risk. However, excessive movement of the scrotum can cause a mechanical inflammation of the epididymis.
What are the symptoms of epididymitis?
Epididymitis is the most common cause of scrotal pain, especially if it comes on suddenly. It can also present with swelling of the scrotum, painful ejaculation, fever and fatigue.
What treatments cure epididymitis?
Treatment is aimed at identifying the cause and treating it. Urinalysis with bacterial testing has replaced, chiefly, the need for swabbing the urethra with a cotton swab. Due to the sensitivity of testing performed by PCR [polymerase chain reaction] or next-generation sequencing, the DNA of the causative bacteria can be identified, and treatment is typically a course of antibiotics. If it is caused by an enlarged prostate, medications, chemical irritation from backflowing urine or excessive activity, those conditions need to be addressed before improvement can be seen.
What preventive measures can men take to encourage the health of the epididymis?
Decrease the risk of infection by supporting general health: controlling sugar if diabetic; using a condom, especially if engaging in anal sex; staying well hydrated; not pushing when urinating—relax, the bladder will push on its own. When bearing down, you can cause retrograde urine flow. See a urologist or your healthcare practitioner for periodic health exams and prostate exams, and use supportive clothing when involved in running, jumping or activities that may cause increased scrotal movement.
How is epididymitis diagnosed?
As mentioned above, urinalysis with PCR or next-generation sequencing DNA bacterial identification is better than a culture that relies on the bacteria to grow out in a petri dish and then be identified. I always tell patients many things can happen to the urine sample from when it leaves your body until the culture is read. Suppose the sample gets too hot or too cold in transportation, leading to false test results. Occasionally, further testing such as an ultrasound or a CT scan of the scrotum may need to be performed. It is also essential to have a physical examination by a healthcare practitioner.
Can epididymitis be acquired without a preexisting sexually transmitted infection?
Yes, since it can happen in boys, too. Non-STI causes include trauma to the testicles, excessive motion of the scrotum, backflow of urine and viruses such as mumps.
Can untreated epididymitis lead to any other conditions?
Untreated epididymitis can lead to more severe infections, such as an abscess, sepsis, scarring and infertility.
How can a man find his epididymis?
The epididymis can be felt by gently palpating the testicles and the tubular structure of the vas deferens. The epididymis lies between these areas.