Treatment and Recovery for Testicular Cancer

If you receive a testicular cancer diagnosis, it is normal to experience a wide range of emotions, from shock and disbelief to concern and fear. You will also likely have a lot of questions about what the diagnosis means for your life. Are there treatments available? What kind? What will it be like going through the treatments? What does recovery from testicular cancer look like? Will life ever be normal again? Will sex be normal?
All of these are valid questions, which your treatment team will answer in detail, but what follows is a general summary of what you can expect.
An overview of testicular cancer
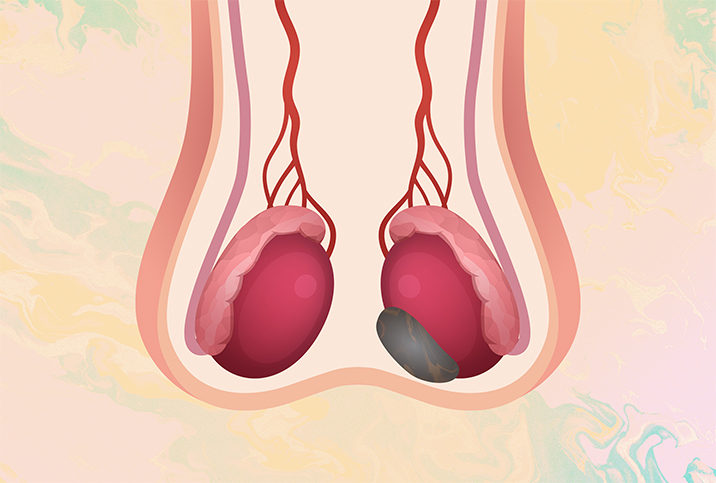
The male reproductive system includes the testicles, typically two of them located under the penis and within the scrotum. Testicles produce testosterone—the hormone responsible for developing masculine characteristics—and sperm.
Testicular cancer develops when healthy cells in the testicles genetically mutate and become cancer cells. Mutations might be inherited, environmental or related to aging. No specific factors for the development of testicular cancer have been identified, but a sharp increase in cases over the last two decades have scientists undertaking new research to determine possible causes.
A rare type of cancer, testicular cancer occurs most often in men in their 20s and 30s. If it is detected and treated early, the odds of a complete recovery are very good.
Surgical treatment for testicular cancer
Treatment of testicular cancer often involves one or more of several types of surgery. Almost all patients, regardless of their cancer's stage, will undergo surgery to remove the cancerous testicle: a radical inguinal orchiectomy. After that, more surgery may or may not be required.
A potential second surgery is the removal of the abdominal lymph nodes, if the cancer has spread to them. This procedure, called a retroperitoneal lymph node dissection (RPLND), is not always necessary; discuss all of your options with your urologist/oncology team. With stage II and stage III testicular cancer, having your abdominal lymph nodes removed may be the best option for a good prognosis, but it is a long and delicate surgery, sometimes carried out with robotic assistance at the surgeon's choice.
Chemotherapy for testicular cancer
Chemotherapy involves the use of powerful drugs—a regimen of bleomycin, etoposide and cisplatin (BEP)—either taken orally (pill form) or given intravenously (IV), to treat cancer. For testicular cancer, chemo drugs are usually given intravenously and the goal of BEP is to shrink tumors and alleviate the signs and symptoms.
It's important to remember that chemotherapy is a systemic approach to eliminating cancer. While the drugs should kill the cancer cells, they may also wreak havoc on the rest of your body in the process.
You should expect to experience some unpleasant side effects, which your oncologist should tell you about prior to treatment. In addition, they will give you detailed information about the drug or drugs being used to treat your testicular cancer, and what to have on hand at home to ease chemo's side effects.
Be sure to go through the list carefully and get all the items you need—these might be over-the-counter or prescribed items—before you go for your first chemotherapy treatment. Some people don't start experiencing chemotherapy side effects until treatment has progressed, but others experience them after the first treatment.
You will go to an infusion center at a local hospital or a cancer center to receive your chemotherapy treatments. The first treatment is likely to be the longest, so be sure to take something to eat and drink with you.
Chemotherapy treatments are administered in cycles, which are repeated several times. A typical cycle is two or three weeks of treatment followed by a week of no treatment, which gives you and your body a little recovery time from the effects of the cancer drugs.
Your blood will be monitored throughout your chemotherapy treatment for testicular cancer. One common side effect of chemo is neutropenia, which is a reduced level of neutrophils, a type of white blood cell manufactured in your body's bone marrow. Neutrophils fight bacterial and fungal infections, so you don't want their numbers getting too low.
Since neutropenia typically occurs between seven and 14 days after chemotherapy treatment, your oncologist may, in the second week of a cycle, order an infusion that gives you white blood cell growth factors. Those factors can help your body make more white blood cells.
Expect to feel fatigued as your chemotherapy treatments progress. You will need more sleep, and you may not have the energy to do much when you are awake. This is a normal side effect of chemotherapy, and it is important to let your body get the rest it needs.
Among the first side effects you may experience with testicular cancer chemotherapy are painful mouth sores. Fortunately, your cancer team will include a palliative care doctor who will be responsible for pain management throughout your treatment and can order a renewing prescription of "magic mouthwash." A custom blend of an antihistamine, an antacid and a local anesthetic that can be swished and spit out or swished and swallowed several times a day, magic mouthwash can significantly reduce the pain and discomfort of mouth sores. It is also helpful against the side effects of nausea and vomiting.
Other common side effects of testicular cancer chemotherapy may include:
-
Hair loss
-
Loss of appetite
-
Diarrhea
-
Easy bleeding
-
Easy bruising
Some less common chemotherapy side effects include neuropathy, kidney or lung damage, hemorrhagic cystitis and loss of hearing.
If testicular cancer chemotherapy is successful, many of the side effects will go away in time, but some may not. There is evidence that suggests men who have completed testicular cancer chemotherapy may develop heart problems as they age.
Radiation treatment for testicular cancer
Radiation therapy for testicular cancer is a targeted treatment for an area of cancer. Radiation is the process of aiming a beam of gamma rays or X-rays at cancer cells to destroy them, and it is commonly used for testicular cancer when the cancer has spread to the lymph nodes.
Before you receive radiation treatment, your oncology team will take precise measurements of the lymph node cancer cells they want to kill, which enables them to angle the radiation beam at the precise location, without damaging any surrounding areas.
While the treatment itself is painless and quick, the setup to get you into the exact position for radiation therapy can take more time, because the beam needs to be aimed so precisely.
Males with seminomas (germ cell tumors that are slow-growing) usually get radiation therapy because seminomas are sensitive to radiation and are more easily destroyed. Radiation therapy may also be used for testicular cancer, both seminomas and nonseminomas (faster-growing tumors), that has spread distantly, to organs such as the lungs, the liver or the brain.
Your oncology team will exercise great care in making sure that as little healthy tissue as possible is affected by radiation therapy. Luckily, the dose of radiation used to treat testicular cancer is typically much lower than that used to treat other types of cancer.
In addition, since radiation can affect your healthy testicle if it reaches it, which in turn can cause fertility problems, your oncology team will place a protective shield over it. The team will also discuss sperm banking with you, in case you and your partner are considering having children in the future.
Though radiation therapy is very targeted—unlike chemotherapy, which is systemic—you can still experience side effects from it, the most common of which include nausea, diarrhea and fatigue. Less common side effects include skin redness or blisters.
As you recover from radiation therapy, the direct side effects will disappear. There may, however, be some long-term side effects, including the possibility that the blood vessels and organs near the lymph nodes could be damaged by radiation, and a higher likelihood that you will develop a second and different kind of cancer as you age.
Recovery from testicular cancer treatment
When it comes to treatments, testicular cancer surgeries will typically take the longest time to recover from, in terms of healing. A radical inguinal orchiectomy can take from two weeks to two months of recovery time. You will not be able to lift anything heavier than 10 pounds for the first two weeks, and you cannot have sex until your incision is fully healed (and your doctor clears you).
You will need to forgo strenuous exercise for at least four weeks, but you should try to walk as much as you are able each day. Most men can resume a good deal of their normal activities within a month.
RPLND surgeries typically have a full recovery time of about two months. You will not be able to lift more than 10 pounds or strenuously exert yourself for about four weeks, but be sure to walk several times a day, to help prevent blood clots from forming, prevent pneumonia from developing and provide relief from constipation.
If your radiation or chemotherapy treatment is successful, you may feel fully recovered in anywhere from two to six months. However, if you had chemotherapy, your recovery time may take up to a year.
Testicular cancer treatment outlook
The recurrence of testicular cancer is infrequent, most likely within 12 months of the first occurrence if it's going to happen, and is usually in the testicle that did not have cancer, so be sure to continue with regular self-exams. Secondary cancers are a long-term concern, so it's important to maintain a regular health and wellness checkup schedule with your primary care doctor.
If your testicular cancer was detected and treated early, your short-term and long-term outlooks are positive. But, as with all stages of testicular cancer, it's important for you to schedule regular appointments with your doctor after your treatment, to help keep you as healthy as possible well into the future.