The Reality of Prostate Cancer Overtreatment

The National Comprehensive Cancer Network (NCCN), a non profit with 32 cancer centers across the U.S. changed its guidelines for the treatment and screening of prostate cancer in September 2021. The new recommendation downgraded "active surveillance" from its perch as the only preferred treatment method for low-risk prostate cancer and added radiation therapy and surgery to the preferred treatment mix. Urologists were not happy.
While it seems like a relatively harmless change, doctors worried it left too much up to interpretation and could lead some to unnecessary intensive treatments in low-risk cases. As a result of immediate and vocal feedback, NCCN reversed the change in December 2021.
But why were doctors so concerned about a change that on the surface seemed to cast a broader net for treating cancer? It doesn't seem like increased treatment for the disease could be a bad thing, but more and more men diagnosed with prostate cancer feel treatment negatively affects their lives more than the cancer itself. Many urologists agree.
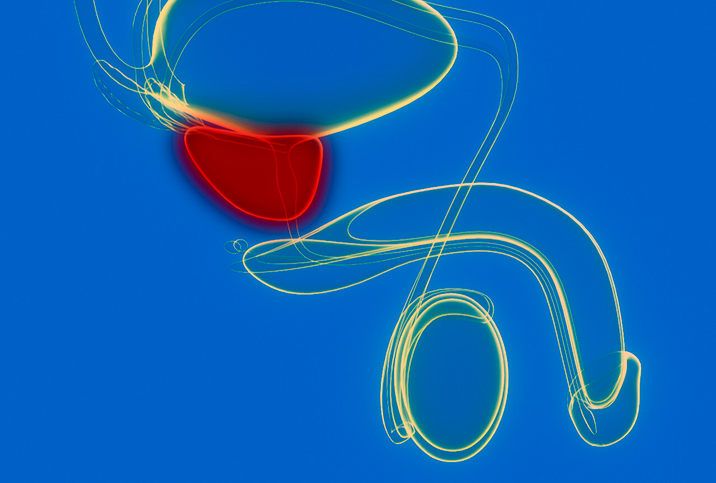
Treating minor cases of cancer with radiation or surgery may cause more harm
While 1 in 41 men will die of prostate cancer, 1 in 8 men will be diagnosed with the disease in their lifetime, according to the American Cancer Society. A 2014 paper published in European Urology noted that prostate cancer overdiagnosis ranges anywhere from 1.7 percent to 67 percent due to screening protocols and doctor's training. The paper suggests that while screening reduces the spread of cancer, overdiagnosis causes more harm. That so many men are diagnosed and so few die is mainly due to increased screening, which often entails blood tests to check prostate-specific antigen (PSA) levels.
PSA levels often rise in the presence of prostate cancer, although high PSA levels can occur for a number of other reasons, including conditions such as prostatitis or benign prostatic hyperplasia (BPH), which has led to the test becoming more of a starting point than the final word. But even in cases where high PSA levels are the result of prostate cancer, rigorous treatment isn't always the right answer. This is why, in cases of low-risk prostate cancer, many urologists prefer active surveillance, which involves frequent PSA testing, digital rectal exams and (in some cases) more detailed testing such as a prostate biopsy, genomic testing and other imaging tests.
"Because other conditions in the prostate can elevate PSA, this tumor marker is not the best in the business for detecting prostate cancer," said Paul Turek, M.D., a reproductive health specialist and urologist with clinics in California. "It is, however, an excellent disease marker to follow prostate cancer once diagnosed."
Unfortunately, the adherence to more frequent testing varies from patient to patient. One 2021 study published in the Journal of the American Medical Association found that nonwhite patients with elevated PSA levels were significantly less likely to receive prostate MRIs than white patients. This lack of standardization even within active surveillance protocols can make it difficult to establish a baseline for treatment modalities. Coupled with the contrasting recommendations and guidelines from organizations such as the NCCN, the American Urological Association, the U.S. Preventive Services Task Force and others, the lack of consensus about testing and treatment leaves a lot of wiggle room for patients to end up receiving treatment they might not need.
"Current guidelines about prostate cancer screening emphasize shared decision-making, which I think is very important," said Stacy Loeb, M.D., a urologist with NYU Langone. While patients should, of course, have a say in their medical treatment, the opinions of medical providers obviously have an outsized impact on how a patient chooses to proceed.
Pressure from clinicians and a lack of information
The inability to partake in shared decision-making can be a result of a number of fears. Patients fear disrespecting their doctor and the fear of feeling responsible in the case of a negative outcome.
In a 2019 peer-reviewed paper published in BMJ, men said they were uninformed about their options and at the same time felt pressured to undergo surgery. Many men in the study were offered few options other than surgery.
"It is crucial that patients are well educated and informed and active participants in this process," Turek said. "Shared decision-making with patients and providers is essential to the success of active surveillance."
"Patients with low-risk prostate cancer can be offered active surveillance. The goal of this approach is to monitor the disease closely over time and to offer curative therapy if there is evidence of progression," Loeb said. "This approach allows many men with favorable tumor features to avoid or delay treatment."
Active surveillance is defined as conservative treatment, whereas active treatment consists of surgery, radiation, hormones and combinations of these approaches. Overtreatment typically refers to active treatment in an asymptomatic patient who is unlikely to develop symptoms or die as a result of prostate cancer.
But what does overtreatment actually feel like?
Side effects of the active treatment of low-risk prostate cancer can include partial or total incontinence, impotence and, in rare cases, death. The emotional or psychosocial impacts of physical treatment side effects such as impotence and incontinence are substantial, while even receiving a diagnosis or undergoing screening can significantly increase anxiety in patients. Several studies indicate that a prostate cancer diagnosis significantly increases the risk of suicide, even in patients with low-risk cases.
On a larger scale, overtreatment of prostate cancer is expensive. NCCN estimates that avoiding overtreatment of low-grade prostate cancer could save the United States approximately $1.32 billion annually.
While overdiagnosis may lead to unnecessary stress and anxiety, expanded screening and testing for early-stage prostate cancer isn't a negative trend. Patients deserve to have the most say possible in their own treatment plans, and the increased knowledge that easier, more accessible testing exists allows patients to become informed about their choices in every stage of treatment.
"There are many new markers and imaging tests for detection and staging," Loeb said. "Many new treatments have also become available. We have also learned a lot more about prostate cancer genetics and are at the beginning of a new era of precision medicine."
Turek said prostate cancer is unique because of its tendency to occur in all people's prostate glands if they live long enough.
"So, because prostate cancer is so common and (early on) slow-growing, it is true that many men will die of other causes even though they have prostate cancer," he added. "In other words, most men die with and not of prostate cancer."
Increasing the accessibility of screening while emphasizing patient education and choice will allow prostate cancer patients to dictate their own future, especially as new technologies develop to simplify screening, active surveillance and treatment as a whole.