Survivors Share Their Post-Mastectomy Surprises
Nicholle Perkins, a now 39-year-old mother and student living in Austin, Texas, was just 22 in 2003 when she was faced with not one but two major life traumas in the span of just a few months.
These events, while significantly different, were intertwined. "I was a manager of a local pizza place in September 2003. and while closing the store down, I was robbed and assaulted by two men," Perkins told me in an interview. "I was thrown on the ground and landed on my right breast with one of the men's weight adding to that impact. The next day, I had a dark blue, almost black bruise, which lasted for a couple of weeks. But, when the discoloration went away, I had a hard lump."
The lump didn't go away. By February, there was dimpling around it. And even though doctors seemed unconcerned, Perkins opted for a lumpectomy rather than the more simple biopsy because the lump hurt—she wanted it out.
Within a week, she got a call and learned the news no one wants to hear: The lump wasn't nothing.
In fact, it was a rare and aggressive form of breast cancer called Triple Negative Breast Cancer. She was sent immediately to Texas Oncology to discuss treatment, and due to her age, the type of cancer, and the size and growth of the tumor, doctors wanted to perform an almost immediate mastectomy.
'My heart sank and I felt sick. I felt like I would never be sexy or attractive to anyone again.'
"At that time, and being only 22, I was overwhelmed with information, not fully understanding or digesting what was being said to me," Perkins explained. "I understood that a mastectomy meant they would remove my breast tissue, but I didn't understand that my nipple would also be removed and that I would have pretty big scars."
The mastectomy was scheduled to be done within a few days, but no one took a beat to talk to Perkins about breast reconstruction or what would be needed to make sure she had the option to reconstruct.
You see, when breast tissue is removed for a mastectomy, placing an implant isn't as simple as going in for an augmentation. Factors like age, body size, scar tissue and skin elasticity can make implant placement more challenging. And due to this, it's advised women who choose a mastectomy have a plastic surgeon accompany them during the procedure to place an expander so reconstruction is possible. This expander helps create the space necessary so an implant can eventually be placed.
With just a few days between her diagnosis and her scheduled surgery, Perkins didn't have a plastic surgeon lined up, and didn't realize she would need one until it was too late. "The night before the surgery, I looked up more info online and learned my nipple would be removed," she recalls. "My heart sank and I felt sick. I felt like I would never be sexy or attractive to anyone again. I lost it. I cried and had a meltdown, my parents cried with me, but what choice did I have? I had to get the surgery."
The next morning in the hospital, lying on the gurney, just before being wheeled into the operating room, Perkins began crying hysterically. "I didn't want to do this. I felt unprepared and was having second thoughts," she said. "One of the nurses squeezed my hand and said, 'Honey, you can stop this and come back next week more prepared. Waiting one week will not be a death sentence. It's okay.'"
That was all the convincing Perkins needed. She stopped the surgery and rescheduled for the following week, which gave her time to line up a breast surgeon and a plastic surgeon to give her greater peace of mind about the procedure. Even so, there was no way to completely prepare for everything the mastectomy would bring.
In addition to a painful recovery from a major surgery, and the change in appearance accompanied by sutures and scars, there were other things Perkins wishes she had known. She, and fellow breast cancer survivors, share their experiences here with Giddy.
Phantom pains sometimes surface, even years later
You may be familiar with the concept of "phantom pains." Generally, it's associated with individuals who have lost an appendage—a finger, leg, foot, or arm—a pain where the limb once existed, but no longer does.
Women who have had mastectomies sometimes feel these pains, too. "I had—still have, but less often—phantom pains where my breast tissue used to be," Perkins said. "It's almost like your body is missing the removed tissue and you feel its pain."
You may experience numbness or cold
Often, oncologists, surgeons and even patients are so concerned with treating the cancer (and understandably so), that patients don't get a full bearing on the types of physical feelings they may or may not have after major surgery.
"I'm often the first person to see a person's breasts other than their surgeon. No one talks to them about how emotionally hard it will be to go forward with a new body," said Beret Loncar, who specializes in post-mastectomy massage at a clinic in Manhattan. "Many have not yet shown their spouses, partners or friends yet, and are scared to."
"No one tells you how irritating the lack of feeling is. Everyone is concerned with pain, but no one talks about the lack of it," Loncar continued. "Nerves are slow healers and while that happens, there can be some weird sensations as things heal. Post-surgically you can be left with areas of numbness or lack of feeling that will drive you a little crazy. It takes time for nerves to heal. Many people find that movement helps but there is also just a period of desensitization to the new sensations."
After undergoing reconstruction, you may be surprised by how cold you feel. With breast tissue removed and implants inserted, the saline, silicone or gummies may always feel chilly against your chest. And because the cold is coming from the inside, it's particularly hard to address. But new inventions are currently hitting the market, including bras and wearable inserts to help keep breast implants warm.
You may wish for a bilateral mastectomy after having a unilateral one
You may assume if there's no obvious reason for a bilateral mastectomy, you're always better off going for the less invasive, unilateral procedure. But now, 17 years after Perkins underwent her unilateral surgery, she wishes she'd done both. Or, rather, she wishes someone would have filled her in on the pros and cons of both options, giving her a fuller picture of what the long-term consequences of one versus the other might look like.
"The biggest reason is peace of mind. I've had several 'scares' because of lumps in my left breast," Perkins explained. "One resulted in surgery to remove the lumps which turned out to be fibroadenomas. This can be a huge source of anxiety. When you've had breast cancer, every lump makes you think it's back."
"The other reason I wish I'd have done both is symmetry," Perkins continued. "Any time I gain or lose weight, my left breast fluctuates in size and the right one stays the same. Also, as I age and gravity is less kind, I'm realizing I'll need more surgery on the left side to keep them more even."
Breast reconstruction isn't a simple, fast or immediate process
Most people think of breast reconstruction and augmentation as more-or-less the same thing. You just go in and place an implant, right? Wrong. Not even close. And what's also important to realize is reconstruction is different for everyone, which is why it's important to get the details from your surgeon and (potentially) plastic surgeon before you have your mastectomy.
"For me, reconstruction started with the expander being placed at the time of the mastectomy," Perkins said. "I went into the plastic surgeon's office every couple of weeks [after the surgery] to have saline injected into the expander so we could slowly stretch the skin to allow for an implant. I did this for several months while going through the chemo treatments. After I finished chemo, I was able to swap out the expander with an implant."
And while Perkins' experience is different from many women's due to her young age, it's been long and intense—and continues to this day. "I've lost count of how many reconstructive surgeries I've had, but it's in the neighborhood of 15, and I have another one coming up in 2022."
That said, she emphasized there have been many advancements since her process started. "The only option I was given was implants, and no matter what type of implant I had (saline or silicone) it didn't look or feel the way I wanted it to," she explained. "On top of that, I had trouble with the implant on the mastectomy side. It capsulated on two separate occasions, resulting in additional surgeries. For the last six years of my reconstruction journey, we've used a combination of a small gummy implant with fat grafting. This option has given much better results both physically and mentally."
Your emotional reaction may be stronger (or different) from what you expect
While making life or death decisions, you may not be thinking too much about your mental health or emotional reactions when your physical health is taking precedence. But removing a part of your body—especially a part our society associates with womanhood and sex appeal—is not something most people can simply accept as a necessary life choice. You are going to have mental and emotional reactions following surgery, and in all likelihood, some will be negative, while others might be positive.
"The period between the mastectomy and initial reconstructive surgeries was pretty terrible," Perkins said. "I was misshapen and the skin looked different than the skin on the rest of my body—it was really tight and shiny. I felt pretty bad about myself physically, [and] then would be hard on myself about being 'shallow.' That period of time was very mentally and emotionally traumatic for me."
On the other hand, Ali Richards, who was diagnosed with breast cancer in 2018, and went through chemotherapy, radiotherapy, hormone treatment and two surgeries, including a mastectomy in 2019, was surprised she wasn't devastated by the physical changes she underwent.
"Having my scar actually makes me feel really strong and powerful," she told me. "Although I'm having reconstruction [in 2021], it really wouldn't be the end of the world if I didn't."
What's important to remember is you will respond emotionally to everything you're going through, and you may be surprised by how you feel. Expect a rollercoaster and seek therapy to help you navigate the ups and downs.
Things might not go as planned, but that might be a positive thing
No one plans to have breast cancer. And when your world is suddenly thrown out of control, you may cling to your treatment plan and its expected outcomes as your only way to control what's happening inside your body.
Unfortunately, there are no guarantees in life, so trying to allow the mental space for flexibility before, during and after your surgery will help you roll with the punches. And in all likelihood, there will be punches.
"I was diagnosed with breast cancer in 2012 at the age of 33," said Jamie Kastelic, a Michigan-based mom and entrepreneur of all-natural hygiene products. "I opted for a bilateral mastectomy, followed by chemotherapy and oophorectomy, and attempted breast reconstruction. However, due to an infection that nearly killed me, I had both breast expanders removed and decided to 'go flat.'"
"Initially, I was devastated," Kastelic admitted. "I wasn't sure how I would move forward and still feel feminine and sexy."
'I wanted other women to see that breast cancer wasn't an 'old lady' disease, but an 'any age' issue. I also wanted people to see that being flat can be a viable and beautiful option.'
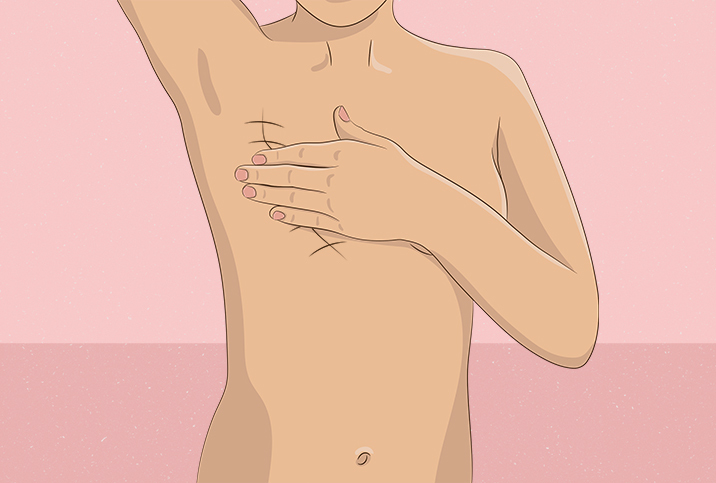
But a series of events helped change her perspective. A local mammography studio needed photos of a woman who had undergone a mastectomy, and they asked Kastelic to model. The plan was to have a picture spanning just from the neck to the torso to help show the different surgical options.
Kastelic agreed to do the shoot, but only if she could show her face. "I wanted other women to see that breast cancer wasn't an 'old lady' disease, but an 'any age' issue. I also wanted people to see that being flat can be a viable and beautiful option."
After the shoot, Kastelic took to social media and posted her flat, bare-chested photos. "The response was overwhelming," she said. "I was one of the first women to share my mastectomy scars to a public audience and since then it has gained traction." And Kastelic herself gained more confidence in her own decision to proudly accept her story and her scars.
The main thing to remember if you're about to undergo a mastectomy is to ask as many questions as you can. Seek recommendations for breast surgeons and plastic surgeons, look for resources for post-surgical therapy of all kinds, and listen to your gut when it comes to making decisions.
It's okay to feel devastated and to wish for things to be different—breast cancer isn't a road anyone wants to walk. Just know many have walked it before you and want to help you navigate the challenges with at least a little more ease than they may have been afforded.