Understanding the 5 Most Common Types of Mastectomies
A mastectomy may be part of your treatment plan if you have breast cancer or are at high risk of developing breast cancer. Understanding your options can help alleviate some of the stress you may be feeling as you prepare for your procedure.
Reasons for a mastectomy recommendation
A mastectomy is a surgery that removes the entire breast. In contrast, a lumpectomy, or breast-conserving surgery (BCS), removes only the cancerous tissue and some surrounding healthy tissue.
A lumpectomy with radiation therapy is often preferred, but a mastectomy may be necessary if you have:
- An inability to undergo radiation treatment
- A genetic mutation, such as a BRCA mutation
- A large tumor relative to the breast size
- A prior BCS with reexcision(s) that were unsuccessful in removing the cancer
- Inflammatory breast cancer
- Two or more tumors in the breast that are far apart
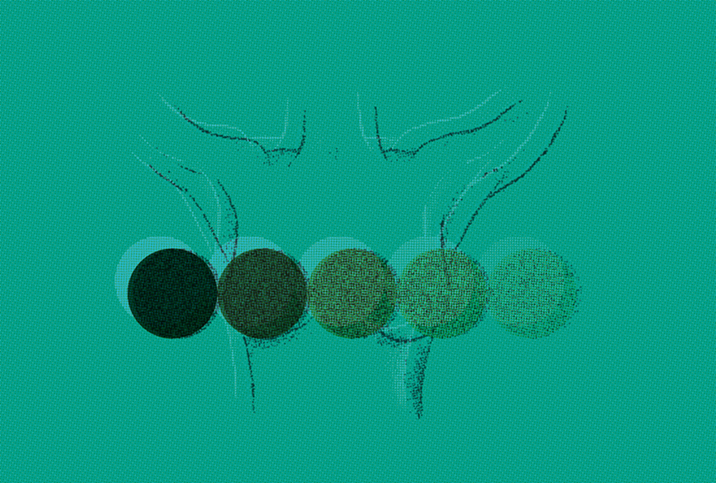
Types of mastectomies
- A simple (or total) mastectomy removes the entire breast, including the nipple, areola and skin. The surgeon may also remove some lymph nodes to test for cancer.
- A skin-sparing mastectomy removes all breast tissue, along with the nipple and areola, but preserves the overlying skin. This less-extensive surgery reduces scar tissue and results in a more natural breast after reconstructive surgery. While many women prefer this procedure, it may not be possible if the tumor is large or close to the skin.
- Like a skin-sparing mastectomy, a nipple-sparing mastectomy leaves the skin intact and attempts to keep the nipple. A small amount of tissue beneath the nipple and areola is removed and examined during the surgery. If cancerous cells are found, the nipple must be removed.
Nipple-sparing mastectomies are best for small, early-stage cancers in women with small to medium-sized breasts. Decreased blood flow to the nipple can occur, causing the nipple to shrink and appear deformed. You may also experience a loss of feeling in the nipple.
Since nipple-sparing mastectomies leave behind more tissue than a simple or skin-sparing mastectomy, the risk of cancer developing may be higher. However, experts feel this can be a safe and effective treatment option in appropriately selected cases.
- A modified radical mastectomy removes the entire breast, nipple, areola and skin, as well as the lymph nodes under the arm. Because cancer can spread from the breast to the lymph nodes and other parts of the body, it is crucial to test the lymph nodes to determine the proper treatment course.
- A radical mastectomy is a complicated surgery, similar to a modified radical mastectomy. The difference is that a radical mastectomy also removes the pectoral (chest wall) muscles under the breast. This procedure has fallen out of favor but may be necessary if the tumor has grown into the pectoral muscle.
Breast reconstruction surgery
It's normal to worry about how your body will look after a mastectomy. Fortunately, breast reconstruction is an option in most cases. A plastic surgeon rebuilds your breast using implants or tissue from another part of your body (or a combination). Reconstructive surgery can be done at the time of the mastectomy or as a separate surgery later.
Mastectomy side effects
After your mastectomy, you may experience side effects, including:
- A buildup of blood or fluid in the wound
- Difficulty moving the arm or shoulder
- Lymphedema (a buildup of fluid below the skin), if lymph nodes were removed
- Nerve pain (burning, tingling, shooting pain, intense itching, numbness) affecting the chest wall, armpit or arm that does not go away (defined as post-mastectomy pain syndrome, or PMPS)
- Numbness in the chest or upper arm
- Pain, tenderness or swelling at the site
- Signs of infection or bleeding
Always keep your doctor in the loop about any unexpected or concerning side effects.
Mastectomy recovery
Most patients need to stay in the hospital for one or two nights, depending on the type of mastectomy. Once you go home, you'll probably need some assistance, but you should be able to resume regular activities within four weeks—longer if you have reconstructive surgery at the same time.
You should be prepared for the emotional impact after surgery, as well, so be aware that a wide variety of support groups are available. Knowing what to expect before your procedure can help you prepare for a recovery that is as safe and stress-free as possible.


















