Can You Get a Pelvic Infection After Egg Retrieval?

In vitro fertilization (IVF) has helped many women conceive. But while the procedure has been a revolution for women experiencing infertility (who can afford it), it is not entirely without complications.
A pelvic infection following a round of IVF is one such complication. Infections are uncommon, occurring in less than 1 percent of all cases, and usually in patients with a previous pelvic infection or endometriosis, according to a 2012 study published in the book "Assisted Reproduction Techniques: Challenges and Management Options."
The risk of getting a pelvic infection is even lower after an embryo transfer. But they do happen, and it's important to know how a pelvic infection can affect your pregnancy so you can watch for the signs.
Possible causes of pelvic infections after egg retrieval or embryo transfer
Pelvic infection and formation of pelvic abscess during an IVF procedure are rare but acknowledged complications of egg retrieval and embryo transfer. The presence of bacterial organisms during embryo transfer or after egg collection appears to be the main culprit.
Contaminated needles and catheters used in the procedure can cause the infection, explained Lori Marshall, M.D., a reproductive endocrinologist, medical director at Pacific NW Fertility and member of Progyny's Medical Advisory Board."An infection after egg retrieval can happen when the needle used for egg collection carries bacteria...toward the abdomen," Marshall said. "It can also occur [when] bacteria from a damaged and previously infected fallopian tube is transferred into the abdomen. When this is severe, antibiotics or even hospitalization might be necessary."
Pelvic infection can also occur after an embryo transfer. "After an embryo transfer, an infection with symptoms of fever and pain is rare, but could occur when the tip of the embryo transfer catheter is contaminated with bacteria, or when the lining of the uterus is already chronically infected," Marshall stated.
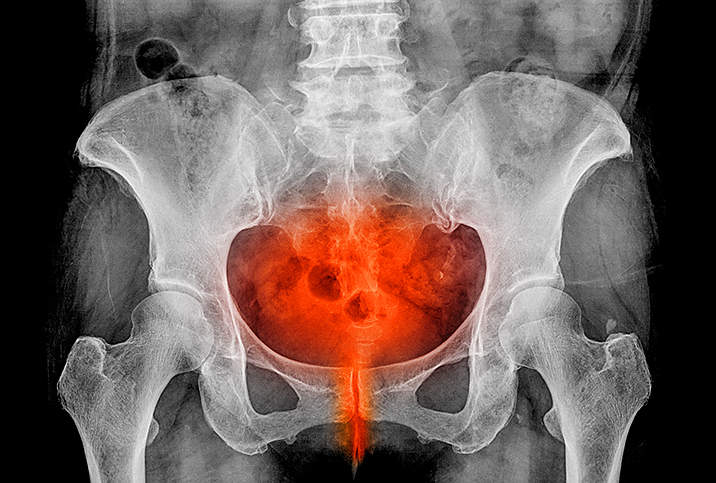
Some of the microorganisms that may cause pelvic infections following an IVF procedure are the same ones that cause pelvic inflammatory disease (PID). Specifically, these are Chlamydia trachomatis and Neisseria gonorrhoeae. The infection occurs when these two bacteria move up from the cervix or vagina and into the uterus, ovaries and fallopian tubes.
In the case of infections caused by these microorganisms within the pelvic region, these may take on the form of a tubo-ovarian abscess. Here, an inflamed mass grows within the fallopian tube or ovary, though in rare cases it may occur elsewhere within the female reproductive system.
Those planning to go the IVF route should expect some pelvic pain associated with the procedure, but infection or abscess will usually cause additional symptoms.
According to James Stelling, M.D., F.A.C.O.G., H.C.L.D., medical and laboratory director of Island Fertility in Commack, New York, gynecologists may look out for the following signs and symptoms in patients being monitored for infections:
- A body temperature (taken orally) higher than 101°F (38.3°C)
- Abnormal cervical or vaginal discharge
- A markedly increased number of white blood cells in the patient's vaginal fluid
- Elevated C-reactive proteins in the bloodstream
Pelvic infections and pregnancy outcomes
It's important to note IVF outcomes depend on a number of factors. However, there is strong evidence pelvic infections that result from bacterial contamination during the IVF procedure can lead to negative pregnancy outcomes.
In a 2012 meta-review of embryo transfer studies, high bacteria levels found in the upper genital tract have been found to negatively impact pregnancy rates after embryo transfer.
Infection of the fallopian tubes, in particular, carries a much greater risk of infertility. Likewise, while pelvic infections can be treated successfully, any scarring that occurs following treatment may further decrease a woman's chances of conceiving and carrying a child to term.
Those planning to go the IVF route should expect some pelvic pain associated with the procedure, but infection or abscess will usually cause additional symptoms.
"If an infection occurs after an egg retrieval, the embryos would be frozen and not immediately transferred until the infection is resolved. After the infection is treated, pregnancy rates should not be impacted," Marshall said. "If there is an infection with or without symptoms associated with an embryo transfer, the implantation of the embryo could be affected and the likelihood of pregnancy will decrease."
Surgery is not usually mandated in the case of infection, but gynecologists may need to drain the pus out of the infected area. In extreme cases, however, surgery is performed in patients with a suspected rupture in either the ovary or the fallopian tube or those whose infections are not responding to the antibiotics.
In severe cases of post-IVF pelvic infection, drastic measures need to be taken in order to halt the further spread of the infection or to prevent a fatality. Such complications tend to occur in women who have had previous pelvic infections or episodes of PID and those diagnosed with endometriosis in the ovaries.
Can complications after egg retrieval or embryo transfer be prevented?
As mentioned previously, infections post-IVF are very rare, but Marshall noted there are ways to reduce the risk of complications further—as well as some things not to do.
"Cleaning the vagina with betadine or other disinfectants to prevent an infection could be toxic to eggs or embryos and is not advised," Marshall warned, "so most fertility clinics use saline to flush away bacteria and vaginal secretions before egg retrieval or embryo transfer.
"Many programs give antibiotics prior to egg retrieval to lower the risk of infection," she continued, "but the risk of infection is so low that it has been difficult to prove that these antibiotics make a difference."
When evidence of a chronic infection of the lining of the uterus is present, Stelling said, antibiotics are usually given, but routine use of any specific antibiotic regimen prior to embryo transfer has not been shown to increase the chance of pregnancy or reduce the risk of infection.
Aside from flushing and antibiotics, women contemplating IVF are usually screened prior to being scheduled for the procedure to ensure they are in the best physical condition for it. A woman's immune system is one key area for screening in order to prevent unnecessary and potentially debilitating complications.
Women with a more robust immune system will have greater chances for a positive outcome than those whose health is compromised by autoimmune disorders, such as lupus and rheumatoid arthritis.
Infection is rare, but be aware of the signs and symptoms
While IVF has helped many women who want children but have been unable to complete a pregnancy, there are a number of complications to consider.
The key lesson here is vigilance. Patients should take the matter up with their gynecologist and learn as much as they can about the procedure as well as any risks it may entail before making their decisions.