Dealing With Antibiotic-Resistant STDs
You've heard of gonorrhea, but how about super gonorrhea? This sexually transmitted disease (STD) got its superpower from slowly but surely building resistance to the antibiotics doctors usually use for effective treatment.
What does it mean when ailments become more powerful than their treatments? And is it a sign of things to come?
What is antibiotic resistance?
"Simply put, antibiotic resistance happens as the direct result of the use of antibiotics," said Manos Perros, Ph.D., president and CEO of therapeutic company Entasis. Perros has a lengthy career in the specialty of infectious diseases and previously worked for AstraZeneca AB as vice president and head of its infection research and early development organization.
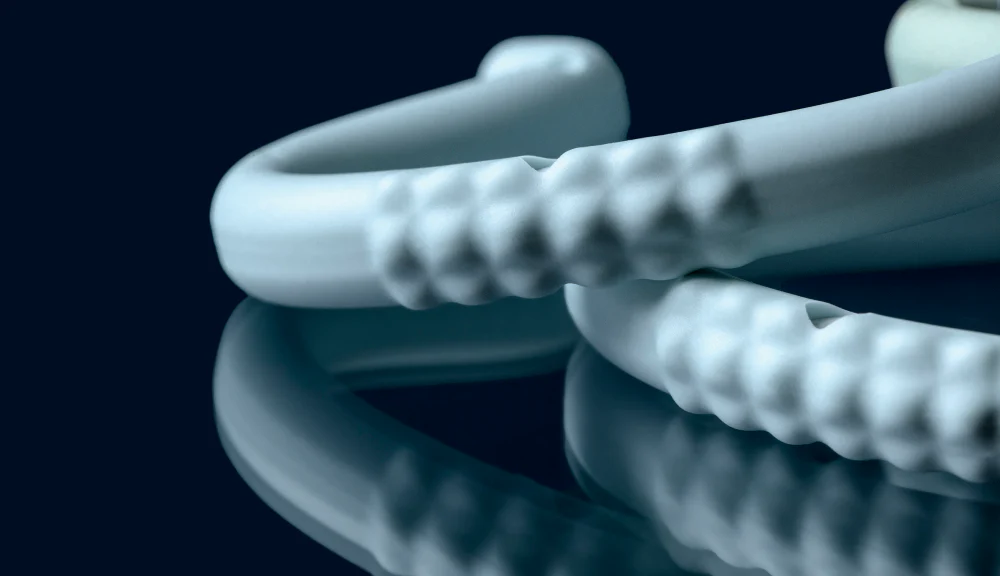
"If you treat a bacterial infection with antibiotics, over time it develops resistance to that antibiotic," Perros explained. "Many STDs, like gonorrhea, are caused by bacterial pathogens. In the case of gonorrhea, the pathogen is called Neisseria gonorrhoeae, and because it is highly transmissible, it has developed resistance to all but one of the antibiotics that have been used historically for treatment."
"Antibiotic resistance is a survival mechanism for bacteria that have evolved as we have used antibiotics to treat infections," added Brian Labus, Ph.D., assistant professor for the Department of Epidemiology and Biostatistics at the University of Nevada Las Vegas.
'If you treat a bacterial infection with antibiotics, over time it develops resistance to that antibiotic.'
"Bacteria have evolved in several ingenious ways to do this," Labus said. "Such as making it harder for the antibiotic to get in; pumping the antibiotic out if it does get in; changing the antibiotic's target; [and] attacking the antibiotic itself. They can also share their approach with other bacteria."
Labus said the overall misuse and overuse of antibiotics has exacerbated the issue, because this allows tougher bacteria to thrive and evolve over time.
"Antibiotic resistance is a problem well beyond [sexually transmitted diseases], with multiple bacteria responsible for infections in the community as well as the hospital," Perros elaborated. "According to the latest estimates, more than 2.8 million antibiotic-resistant infections occur in the United States each year, with over 35,000 Americans dying from them (likely an underestimate, as most of these infections are not reportable)."
How common are antibiotic-resistant STDs?
"Due to the frequent overuse and misuse of antibiotics when treating STDs, antibiotic resistance is becoming more common," said Sherry Ross, M.D., a women's health expert and author of "She-ology: The Definitive Guide to Women's Intimate Health. Period."
"According to the latest estimates from the Centers for Disease Control and Prevention (CDC), 1 in 5 Americans has suffered from sexually transmitted infections (STIs), with 26 million infections acquired in 2018 alone," Perros added. "It would be fair to say that today, most of these STIs are resistant to one or more antibiotics."
"Resistance is more common for some infections than others, and that has forced us to change our treatment guidelines," Labus said. "We stopped treating gonorrhea with penicillin in the 1980s because of antibiotic resistance, but it is still our go-to treatment for syphilis because it is still highly effective. Unfortunately, gonorrhea has developed resistance to every antibiotic we have used to treat it except ceftriaxone. We are basically out of other options and need new treatments."
"The [STDs] of most concern are those caused by bacteria which are called 'multi-drug resistant,'" Perros added. "To put it plainly, these are bacteria that have developed resistance to multiple antibiotics, leaving us with few or no therapeutic treatment options. A good example is gonorrhea."
This growing antibiotic resistance is concerning for several reasons, some with more long-term consequences.
"Syphilis, gonorrhea, and chlamydia are three [STDs] that have shown signs of antibiotic resistance," Ross said. "If [STDs] become entirely resistant to antibiotics, this could be catastrophic to women's reproductive health and our future fertility."
Treating antibiotic-resistant STDs
"Luckily, in the U.S., the majority of [STDs] are still treatable by mainstream antibiotics," Perros said. "But, there are multiple cases of 'untreatable' gonorrhea around the globe, in particular Southeast Asia and the Pacific, but with a growing number of reports in Western Europe and more recently in the U.S.
"If you contract one of these, you're a subject for salvage treatment," Perros continued. "This is where physicians reach out for combinations of antibiotics, potentially requiring multiple injections or infusions to control the infection."
According to Perros, the antibiotic ceftriaxone is the last line of defense at present, and the CDC recently doubled the recommended dose from 250 milligrams to 500 milligrams. Despite the double up, the dosage is actually higher in other parts of the world, indicating the antibiotic is not a long-term solution.
"So, yes, treatment does have to change," Perros explained. "We need newer, more potent antibiotics which work against multi-drug resistant infections and which ideally can be administered orally."
Addressing the problem
"The most important thing we can do is prevent infections in the first place through safe sexual practices," Labus said.
"Many [STDs] are preventable if adequate protection is used during sexual intercourse," Perros said. "In addition, [STD] screening not only helps a patient get timely treatment but also prevents them from infecting others."
Labus went on to again stress an evaluation of how we use antibiotics to prevent future resistance. The basic steps he suggested are finishing the entire prescription, even if you're feeling better, and not taking the antibiotic for anything other than what your doctor has advised.
"We also work extensively with healthcare providers," said Labus. "This is to make sure that they are always kept up-to-date on our [STI and STD] treatment guidelines so that we can do our best to prevent resistance."
In order to stay ahead, all patients, doctors and pharmaceutical companies will have to work together in stemming potential waves of resistance.
Behind the scenes, scientists are working to develop new ways of treating antibiotic-resistant infections.
"Even for those who contract an antibiotic-resistant [STD], there's still good news," Perros said. "Antibiotic-resistant bacteria are tough adversaries, but we know how to defeat them. We've done it for decades."
The pharmaceutical industry, too, is on top of it, and exciting breakthroughs are on the horizon.
"At Entasis, we have a new oral investigational antibiotic, zoliflodacin, which is currently in late-stage clinical trials against gonorrhea," Perros added. "It has been shown to work equally well against both drug-sensitive and antibiotic-resistant infections in the laboratory. We are working with our partners to conduct a global clinical trial which, if successful, could lead to approval and commercialization of the first new class of antibiotics for gonorrhea in decades!"
In order to stay ahead, all patients, doctors and pharmaceutical companies will have to work together in stemming potential waves of resistance.
"I believe that this may lead us to a safe and effective oral option treatment for patients with gonorrhea," Perros explained. "And that's what matters most. We need more of these to stay ahead of the problem."