Let's Talk About Oral Allergies
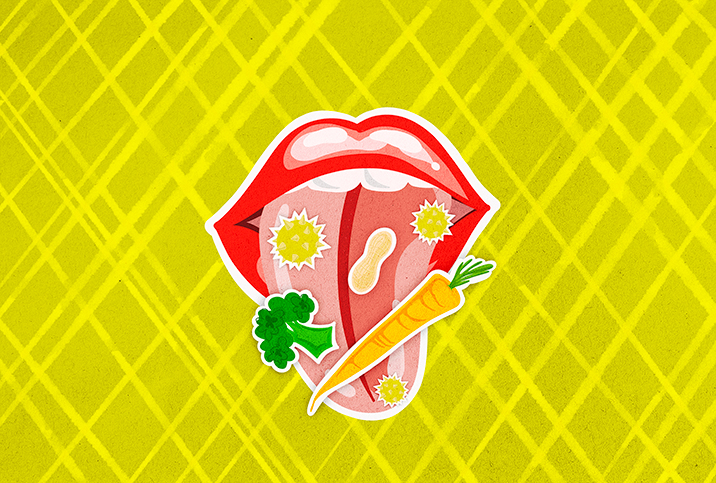
In the past few decades, more people are discovering they have allergies triggered by all kinds of environmental factors and food. Oral allergy syndrome (OAS) is one such condition, and it's often misdiagnosed.
The American Academy of Allergy, Asthma and Immunology defines oral allergy syndrome (also known as pollen food allergy syndrome (PFAS)) as a form of a contact-allergic reaction, which occurs upon contact of the mouth and throat with raw fruits or vegetables.
"Certain foods that have similar proteins to pollen trigger an immune reaction that may cause itchiness and discomfort in the mouth," explained Priya Bansal, M.D., faculty member at Northwestern University Feinberg School of Medicine. "For example, someone [who] is allergic to birch pollen may find that their tongue swells or gets itchy when they eat a peach. This may occur with different foods in patients allergic to grass pollen and weeds as well."
Oral allergy syndrome 101
There are a variety of different allergies that all manifest differently. Maddy, from Seattle, didn't recognize her condition initially, thinking she simply experienced excessive allergy symptoms.
"I thought it was an adult-onset tree nut allergy," Maddy said. "Then, after nuts were eliminated and the problem was still ongoing, I realized it was oral allergy syndrome."
Even as a self-proclaimed medical nerd, she never considered oral allergy syndrome as a possible diagnosis.
Bansal described the symptoms of oral allergy syndrome as "itchiness within the mouth and swelling of the tongue, throat, mouth, lips and face, usually occurring after exposure to raw fruits and vegetables, and can in rare cases lead to a severe allergic reaction, what we call anaphylaxis."
Certain foods that have similar proteins to pollen trigger an immune reaction that may cause itchiness and discomfort in the mouth.
It may only be certain fruits and vegetables, without all of them related to a particular pollen. Patients who have oral allergy syndrome are usually diagnosed by having a positive skin test and symptoms consistent with the diagnosis.
For Maddy, that was "an itchy and swollen mouth, a pickaxe buried in my head and then so much pressure in my sinuses that I wanted to pull out my molars, followed by what felt like a kidney stone trying to pass in my nasal cavity. It also came with a ton of brain fog."
Her diagnosis took longer than a year, including an MRI to rule out a brain tumor since her patch tests came back negative. Negative patch tests are not unusual, but her allergist was unfamiliar with oral allergy syndrome and didn't know what other clues to check for.
Treatment and management
Peculiar to oral allergy syndrome is the fact that it affects each person uniquely.
For example, someone who is allergic to birch tree pollen—an allergy prevalent during springtime—may have reactions triggered by pitted fruit or carrots. People with allergies to grasses may have a bad reaction to peaches, celery, tomatoes, melons (cantaloupe, watermelon and honeydew) and oranges. And anyone who has a reaction to ragweed might present symptoms when eating bananas, cucumbers, melon or zucchini.
People who have already been diagnosed with allergic rhinitis—an inflammation of the inside of the nose—or have an allergy to multiple pollens may be at a higher risk of oral allergy syndrome.
Avoiding triggers is key to managing most allergies, but with oral allergy syndrome, it's best to avoid provoking anything that might risk anaphylaxis. Bansal recommends avoiding "all trigger foods, especially during the pollen season."
When a reaction occurs, over-the-counter medications like antihistamines may help. Oral allergy symptoms that manifest as itching, watery eyes and scratchy throat can be treated with diphenhydramine (Benadryl) and fexofenadine (Allegra). Some people who have had immunotherapy—a biological therapy to activate or suppress your immune system—may notice an increased tolerance for birch pollen, but this will not overcome oral allergy syndrome.
Know your triggers
The biggest advantage in fighting a diagnosed allergy is knowing what your triggers are. Maddy emphasized her "constant vigilance" in managing her condition, insisting that being strict about diet is key. "Even the residue from a cherry placed on some whipped cream will lead to intense pain," she explained.
"Heating the food at a high temperature (such as baking it) may denature the protein and decrease the reaction," Bansal said. "Peeling the food prior to ingestion may also ease symptoms by decreasing the amount of protein that contacts the mouth. If systemic symptoms are seen consistent with anaphylaxis, it is important to carry an epinephrine auto-injector in case of accidental ingestion." Other precautions can include buying canned vegetables and fruits.
A small percentage of people with oral allergy syndrome will experience severe symptoms that require medical assistance. Since it is easy to confuse serious nut allergies with oral allergy syndrome, if you suspect you may have this condition, it is important to see your primary care physician as soon as possible for official diagnosis and treatment.


















