A Primer on Monkeypox and Pregnancy

Monkeypox, an endemic virus in certain parts of Africa, hasn't often been seen in Europe and the United States until recently. Since May 2022, cases of the dangerous virus have been rising, and people looking to start a family may be worried about their safety.
Here's what you need to know about monkeypox and pregnancy.
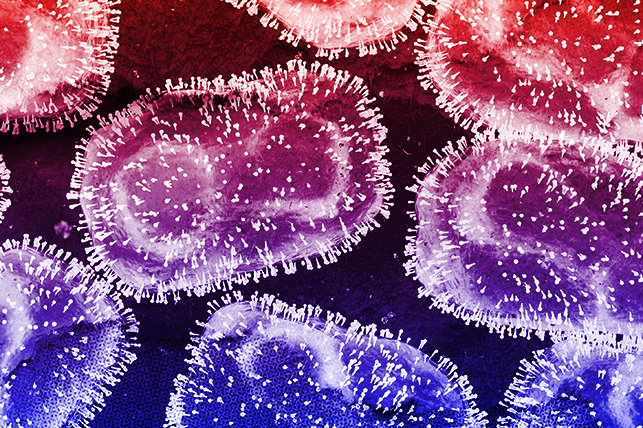
What is monkeypox?
The monkeypox virus is part of the same family of viruses as smallpox. The symptoms are similar to smallpox, presenting as fever, swollen lymph nodes, headache, respiratory issues and a painful blister-like rash, according to the Centers for Disease Control and Prevention (CDC). The rash can appear across the body, including the mouth, genitals and anus.
Symptoms of monkeypox present similarly in pregnant people as in the general population. However, other rashes can occur during pregnancy, so your physician will have to order tests to rule out sexually transmitted infections (STIs), shingles and other common skin conditions.
Monkeypox can be spread to the fetus through the placenta and direct contact. At this time, it's unknown if the virus can spread through breastfeeding.
How monkeypox affects pregnancy outcomes
Data on monkeypox and pregnancy outcomes are scarce. It's unknown if pregnant people are more at risk for contracting the virus or if the virus is more severe during pregnancy, according to the American College of Obstetricians and Gynecologists (ACOG).
Only five laboratory-confirmed cases of monkeypox and pregnancy have been documented, according to a July 2022 article published in the journal Obstetrics & Gynecology. Of these cases, three pregnancies resulted in fetal loss, including two spontaneous abortions (miscarriages) and one stillbirth. The fourth case resulted in a full-term pregnancy and the infant was healthy with no signs of monkeypox. In the fifth case, the infant was born preterm and had a rash, possibly due to monkeypox infection, though no tests were available to confirm. The infant later died at 6 weeks of age from malnutrition. It's important to note that all of these cases occurred in African countries. There is currently no data on U.S. women.
No data are available on whether cesarean birth should be recommended for people with monkeypox. Transmission timing and rates are unknown. However, a C-section may be offered in cases where the mother is presenting with genital blisters to reduce contact with the baby and potentially decrease the risk of transmission.
Postpartum considerations
New mothers presenting with monkeypox symptoms are recommended to avoid handling their newborns until their lesions have resolved and a new layer of skin has formed, according to ACOG. While the benefits of skin-to-skin contact for newborns have been demonstrated at length, transmitting the virus and potentially causing severe illness in your baby is a real risk.
While it's unknown if monkeypox can be spread through breast milk, breastfeeding should also be delayed until lesions are gone. It's recommended mothers pump and dump until new skin is formed and their doctor clears them to breastfeed.
Separating from your newborn can be emotionally difficult for new moms. While avoiding close contact is recommended, the CDC has provided guidelines for mothers with monkeypox who choose to have contact with their babies:
- No skin-to-skin contact.
- The newborn should be swaddled or clothed during contact.
- After contact, the newborn's clothing and/or blankets should be changed.
- The mother should wear gloves, fully covered clothing and a medical mask during contact.
Treating and preventing monkeypox in pregnant people
The good news is that pregnant people can be vaccinated against monkeypox. If you're at high risk for infection, your doctor may recommend vaccination. Postexposure vaccination is also an option; ACOG recommends getting vaccinated within four days of exposure for maximum protection.
The two available vaccines are ACAM2000 and JYNNEOS. ACAM2000 is not recommended for pregnant people because of an increased risk of pregnancy loss, congenital defects and virus infection in newborns. JYNNEOS, however, can be administered to pregnant women. There is no data on the safety of this vaccine in people who are pregnant, but animal studies have shown no evidence of harm to the fetus.
The safety of the JYNNEOS vaccine has not been studied in breastfeeding women, but according to ACOG, it should not present a risk of transmission through breast milk.
Treatment for monkeypox is also available for pregnant and breastfeeding women. Patients are first and foremost recommended to isolate at home until they are cleared to be around other people again.
There are several safe medicinal treatments, but the first line of defense is tecovirimat, an antiviral. Alternatives include the antivirals cidofovir and brincidofovir. Your doctor can prescribe the best medication for your situation.