How Do You Know If You Have Monkeypox?

The highest number of monkeypox (mpox) cases in the world is reported in the United States, with a total of 30,225 cases, according to the Centers for Disease Control and Prevention (CDC). As of March 1, 2023, 38 deaths had been recorded.
Transmission of the virus has been shown to occur through physical contact during anal, oral and vaginal sex. Complications of mpox include confusion, eye issues and pneumonia, as well as proctitis, which causes painful sores and swelling inside the rectum. Mpox can be transmitted to the fetus during pregnancy or to a newborn during and after birth. Cases of spontaneous pregnancy loss and stillbirth have been recorded in some cases of confirmed mpox infection.
Here are some signs that can help you recognize and identify the disease.
Common symptoms
"Mpox is a virus that causes a fever, fatigue, headache and muscle pain," said Brittany Kmush, Ph.D., associate professor of public health at Syracuse University in New York. "A few days after these symptoms start, a rash appears that can look like chickenpox, smallpox or measles. However, mpox is usually also accompanied by swollen glands. Mpox infects humans as well as other primates and rodents."
Suraj Saggar, D.O., chief of infectious disease at Holy Name Medical Center in Teaneck, New Jersey, illustrated the rash much more vividly.
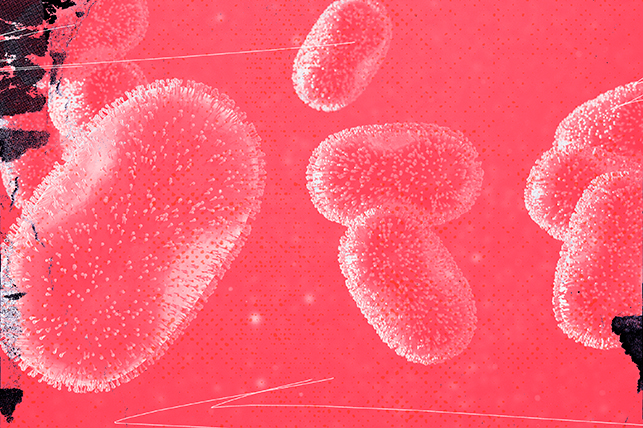
"Clinical signs and symptoms [include at] first flu-like syndrome—fever, chills, body aches—then genital, anal and/or oral lesions. [It] can look like an STD," he said. "The rash has several stages, starting as 2 to 5 millimeters macules and evolving into vesicular lesions that then crust over and dry out."
A macule lesion is a flat, discolored patch of skin. Despite the name "lesion," a macule shouldn't hurt. To give you a frame of reference, tattoos and freckles technically qualify as macules, too. A vesicular lesion, or vesicle, is much more troublesome. These fluid-filled sacs just beneath the top layer of the epidermis more closely resemble what we think of as blisters.
Diagnosis and testing
Kmush introduced in large strokes the components needed to obtain a diagnosis of mpox.
"Mpox can be diagnosed based on the signs, symptoms and a connection with a mpox case," she said. "Viral testing from the skin lesions using polymerase chain reaction [PCR] is used to confirm the diagnosis."
Manoj Gandhi, M.D., Ph.D., senior medical director of Thermo Fisher Scientific in San Francisco, delved further to differentiate between probable cases and confirmed cases. Eyeballing this rash can cause confusion. Based on placement across the body and the severity, the condition can be mistaken for chickenpox or even a sexually transmitted infection (STI).
"The CDC has defined specific guidelines for the diagnosis of mpox," he explained. "This is based on the clinical presentation of the patient as well as the laboratory findings. The patient can be defined as 'suspect' and/or 'probable' if there is reasonable clinical suspicion of an unexplained rash and/or positive Orthopoxvirus lab test result. However, a 'confirmed' diagnosis is provided only if there is a positive PCR result or if the virus is cultured from a clinical specimen. Since it may not always be possible to distinguish an STI lesion from a mpox lesion or a chickenpox rash from a mpox rash, a confirmatory test such as PCR is the only way to confirm mpox."
When to seek help
Gandhi noted that in cases of interspecies viruses (such as mpox), isolation considerations should be extended to every single housemate, human or animal.
"If a person suspects infection with mpox, they should seek care and get tested," he recommended. "If indeed they are positive for mpox, they may be candidates for treatment with antivirals such as tecovirimat [brand name: Tpoxx]. These patients should exercise good judgment to prevent the spread to others, such as self-isolating until the rash has healed, not sharing things with others, cleaning and disinfecting at home, notifying their close contacts so that they can look out for symptoms and getting tested, and even limiting contact with pets as the virus can infect animals."
Yes, even cats and dogs are at risk, so temporarily boarding your furry friend at a kennel, with your veterinarian or with a loved one may prove the safest and most convenient decision. Since the virus is contained in the fluid of the scabs, a game of tug-of-war, an overexcited greeting or a misplaced cat scratch could easily segue into a contamination risk.
What happens if it goes undiagnosed?
Brian Labus, Ph.D., M.P.H., assistant professor of epidemiology at the University of Nevada, Las Vegas, described the timeline of how an infection should look for an otherwise healthy individual.
"For most people, the outcome really isn't any different, as the virus has to run its course whether it's diagnosed or not," Labus said. "The big difference is that the infected person won't know that they need to take steps to prevent spreading the disease to others. For people at high risk of severe disease, there are some experimental treatments available that require a diagnosis. Your body usually fights off a mpox infection after two to four weeks and it doesn't cause long-term symptoms."
Kmush said the situation may be more dire for immunocompromised patients and the very young or very old.
"If you suspect you have mpox, visit your healthcare provider," Kmush advised. "There are some medications that can lessen the severity of the infection. People who you live with are at risk of developing the infection, so you should isolate away from other people. Most people will recover from mpox, but young children and those with HIV or other immune-compromising conditions are at higher risk of developing secondary infections, other complications and death."
The risk from these factors—preexisting illness and age—extends to any pets you have.
Treatment options, side effects and costs
Labus noted that one upside to mpox's familial resemblance to smallpox—despite the virus's differences—is that they share the same vaccine.
"The vaccine for mpox is based on the vaccine we use against smallpox, as they are closely related viruses," Labus said. "It is available for people at high risk of infection or those who have been recently exposed to someone with mpox. All vaccines can have side effects, the most serious of which is a rare but severe allergic reaction to one of the vaccine components. For most people, the side effects of mpox vaccination are mild and include pain or soreness at the site of injection, fatigue and fever."
Risk management is often a heavy consideration for people with histories of strong allergies to vaccines, but thankfully, such cases among the general public are rare.
Labus explained that less severe cases might require a trip to your local drugstore or the use of what's already in your medicine cabinet.
"Unfortunately, there isn't much that people can do to reduce the severity of mpox. It has to run its course," he added. "That doesn't mean there isn't anything you can do to feel better. Medicines like ibuprofen or acetaminophen may help manage the pain that often comes with the rash, and over-the-counter medications like topical benzocaine/lidocaine gels, oral antihistamines, calamine lotion or warm baths may help reduce the itching caused by the rash."
A case of mpox may require time off from work, which isn't always a realistic option for everyone. Isolation, rest and recovery is really the only way to prevent the condition from worsening and spreading.