Monkeypox: Moving Beyond the Basics
Often mischaracterized as a sexually transmitted infection (STI), monkeypox—now renamed mpox by the World Health Organization (WHO)—is a painful but generally nonlethal relative of smallpox.
The mpox virus can be passed to someone via physical contact during anal, oral and vaginal sex. Complications include confusion, eye issues and pneumonia, as well as proctitis, which causes painful sores and swelling inside the rectum.
The virus can be transmitted to the fetus during pregnancy or to a newborn during and after birth. There have been reported cases of spontaneous pregnancy loss and stillbirth in some cases of confirmed mpox infection.
Impacting sexual health
Manoj Gandhi, M.D., Ph.D., senior medical director of Thermo Fisher Scientific in San Francisco, assigned parameters to mpox around sexual behavior, but the caution extended beyond intercourse.
"Mpox is often transmitted through close, extended physical contact which occurs during sex," Gandhi said. "If someone is at high risk for mpox, they should consider getting vaccinated against it and temporarily change parts of their sex life until they are fully vaccinated. If mpox infection is suspected, the best approach is to avoid sex of any kind with people who have symptoms that indicate mpox infection and especially avoid touching any rash. Avoid or limit sharing any personal items, and do not attend any gathering such as rave parties, saunas, sex clubs, or private and public sex parties."
While "personal items" may mean dildos, cock rings and other sex toys, there are plenty of nonsexual items known to transmit germs if shared. For example, Chapstick, makeup brushes and water bottles are all benign items that are fine to give to people but not to share in the case of mpox.
Complications and related conditions
Severe and untreated cases of mpox can turn into encephalitis, a neurological infection causing swelling of the brain that may compromise vision; pneumonia is another common complication.
The rate of mpox fatalities in the United States is low compared to the rest of the world: 38 deaths among a reported 30,262 cases as of late March 2023. Aside from tragic ends to the very rare severe cases, mpox doesn't seem to cause "long hauler" complications, making it different from experiences with COVID-19.
As far as related conditions, certain individuals are advised against receiving the mpox vaccine. These more vulnerable populations include pregnant mothers, those with certain skin or autoimmune disorders, cancer patients, organ transplant patients and a few other medically compromised groups.
Living and dating with mpox
Brittany Kmush, Ph.D., associate professor of public health at Syracuse University in New York, explained that the greatest problem for people with mpox casually dating is the asymptomatic cases.
'It's important to become familiar with symptoms so transmission scenarios can be avoided.'
"Some people with mpox do not develop any symptoms at all," she said. "The initial symptoms of mpox resemble the flu, with fever, fatigue and headache. It is the rash, which develops a few days after these initial symptoms, that distinguishes it from the flu. A healthcare provider can determine the cause of the rash and other symptoms, as several other illnesses—including chicken pox and measles—can look similar to mpox."
As asymptomatic mpox does exist, the message is to get tested.
Prevention, aftercare and resources
"A human can get infected with mpox from contact with an infected animal or human," Kmush explained. "They can get infected if infectious viral particles come in contact with broken skin, the respiratory tract, the eyes, nose or mouth. There is also evidence that mpox can be transmitted from sexual contact. People living with or caring for someone with the virus are most at risk of developing mpox."
Prevention may involve bandaging small open wounds, requesting an mpox test at the veterinarian or being extra zealous about basic hygiene. Masking and wearing goggles in high-risk situations can discourage transmission. Moisturizer and aloe vera gel can also prevent the open wounds through which the virus spreads.
"You should follow general infection prevention practices, like not sharing utensils and handwashing," Kmush suggested. "There is a vaccine to prevent mpox. Those caring for someone with mpox should receive the vaccine as well as wear personal protective equipment. Someone infected with mpox should isolate away from others to prevent spreading the illness."
It's important to become familiar with symptoms so transmission scenarios can be avoided.
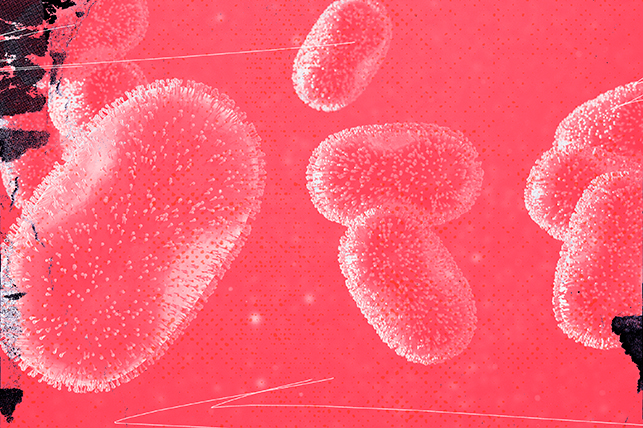
"The most classic presentation of mpox is a rash that starts on the face and spreads to the rest of the body," Gandhi explained. "The rash progresses through its course, developing into pus-filled blisters followed by ulceration, scabbing and spontaneously healing. However, what has been observed in this outbreak is that the rash often occurs as isolated lesions around the private parts and resembles an STI. As a result of this clinical presentation, a lot of the mpox patients are first seen in STI clinics. In addition to the rash, patients may also exhibit nonspecific symptoms such as fever, chills, swollen glands, body ache, etcetera, but these can vary widely."
Consequently, the best strategy is to get tested at an STI clinic. What you think may be a case of herpes could easily be mpox.
Don't plan for an activity-filled day after receiving the vaccine. Clean bedding and even temporary abstinence from sex is recommended even if that means waiting a full month until you've received both doses of the vaccine.
What is the future of mpox?
Brian Labus, Ph.D., M.P.H., assistant professor of epidemiology at the University of Nevada, Las Vegas, addressed the big question on everyone's lips: Could mpox become another pandemic like COVID-19?
The good news is the scenario is unlikely.
"There are types of mpox called clades," Labus explained. "The clade causing the current outbreak is clade IIb, which spreads more easily in humans but also has a very low death rate. We have seen a continual decline in the number of cases since early August [2022] thanks to vaccination and behavior change, so we are not seeing any indication that the outbreak is trending upward."
Unlike COVID-19, mpox is not an airborne virus. The preexistence of a suitable vaccine is also a major help. The smallpox vaccine available now is based on medicines first developed more than 200 years ago.
The vaccines are seen as a silver lining to a very uncomfortable cloud. While the future for curing mpox looks hopeful, caution and cleanliness are still solid strategies.